Unlocking NIH Stroke Scale: Key Principles Deciphered
Explore the essential principles of interpreting NIH Stroke Scale scores. Gain insights crucial for assessing stroke severity, empowering healthcare comprehension.
In the realm of healthcare, a pivotal metric that stands as a linchpin in the assessment of stroke severity is the NIH Stroke Scale (NIHSS) score. Understanding this numerical evaluation is fundamental in deciphering the extent of neurological impairment resulting from a stroke. This article serves as a compass, navigating through the intricate landscape of healthcare topics, with a dedicated focus on unraveling the intricacies of the NIH Stroke Scale score. Delving into the intricacies of its key principles, we aim to equip readers with a comprehensive understanding of this standardized assessment tool. In this pursuit, clarity and objectivity will guide our exploration, avoiding the pitfalls of subjective interpretations. As we embark on this informative journey, it is paramount to recognize the NIH Stroke Scale score as more than a mere numerical figure, but as a critical compass directing healthcare professionals toward a nuanced comprehension of stroke severity.
Top 10 Points about Key principle to remember about a NIH Stroke Scale score. :
- Decoding the NIH Stroke Scale: Unveiling Its Significance
- Understanding Neurological Impairment: A Closer Look at NIHSS Scores
- The Core Principles: Foundation of NIH Stroke Scale Assessment
- Interpreting Stroke Severity: Navigating the NIHSS Landscape
- Crucial Insights: What Every Healthcare Professional Must Grasp
- Key Components of NIHSS: Breaking Down the Assessment
- Why NIH Stroke Scale Matters: Insights into Comprehensive Evaluation
- Mastering the Basics: NIHSS Score as a Fundamental Diagnostic Tool
- Practical Application: Integrating NIH Stroke Scale in Clinical Settings
- Beyond Numbers: NIHSS as a Window into Stroke Complexity
Several facts about Key principle to remember about a NIH Stroke Scale score.
Introduction
Welcome to the intricate world of healthcare, where the NIH Stroke Scale (NIHSS) score emerges as a pivotal tool in understanding and assessing stroke severity. This article endeavors to unravel the key principles that underscore the significance of this numerical evaluation, shedding light on its importance in the realm of neurology.
The Foundation of Assessment
At the core of stroke evaluation lies the NIH Stroke Scale's key principles. Understanding the foundation of this assessment tool is crucial for healthcare professionals tasked with deciphering the neurological impact of strokes. It serves as a comprehensive guide, ensuring a nuanced comprehension of the patient's condition.
Decoding Neurological Impairment
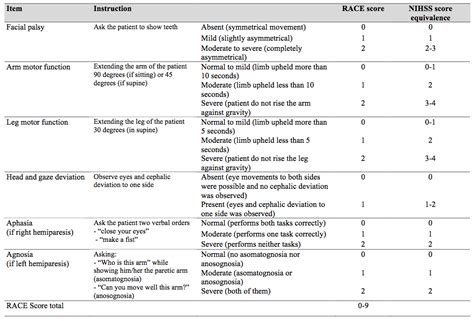
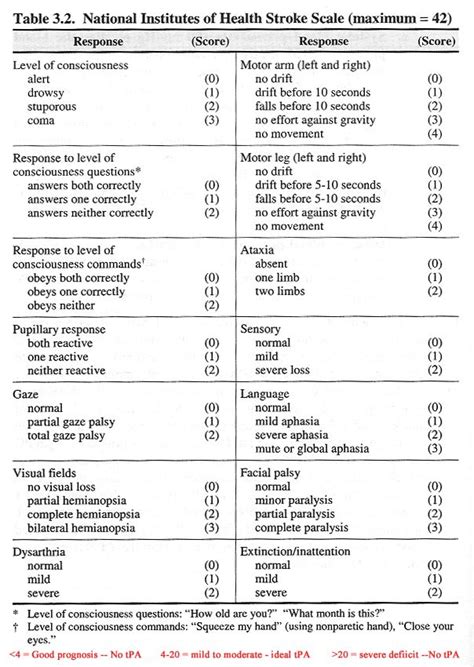
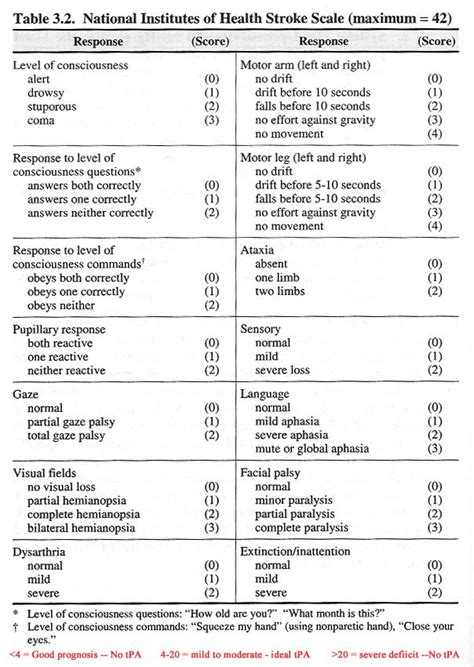
Delving deeper, we uncover the nuances of neurological impairment through the lens of NIHSS scores. Each element of the scale contributes to the holistic understanding of the patient's condition, allowing healthcare practitioners to tailor their approach based on specific impairments identified during the assessment.
Practical Application in Clinical Settings
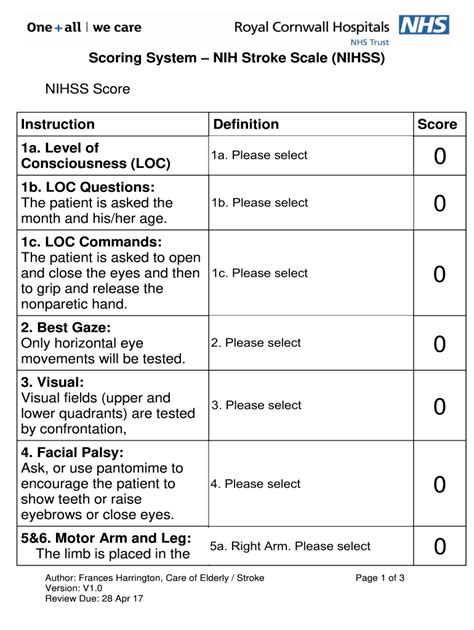
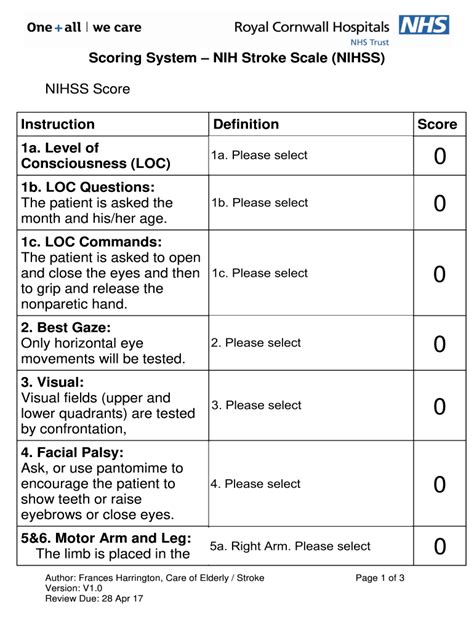
Bringing theory into practice, the NIH Stroke Scale finds its application in clinical settings. Healthcare professionals utilize this tool to make informed decisions, ensuring that patients receive timely and appropriate interventions based on the severity of their neurological impairment.
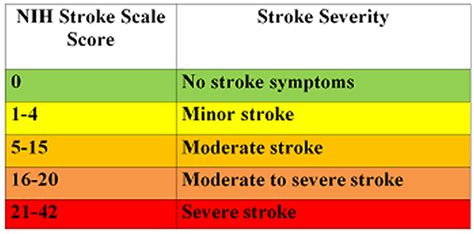
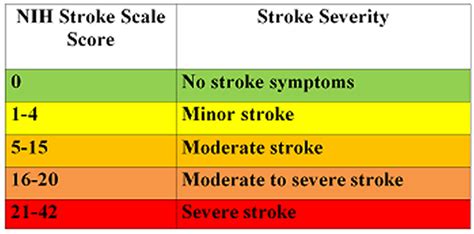
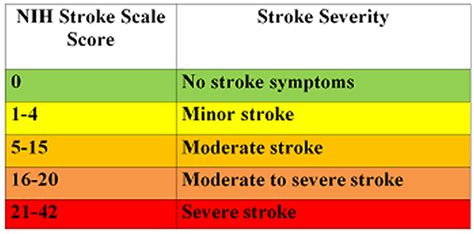
Interpreting Stroke Severity
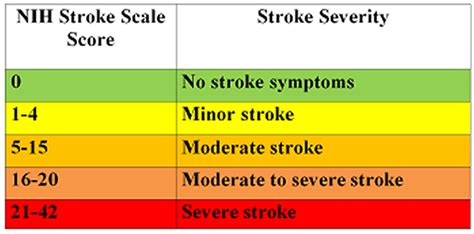
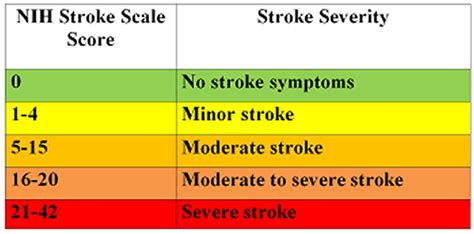
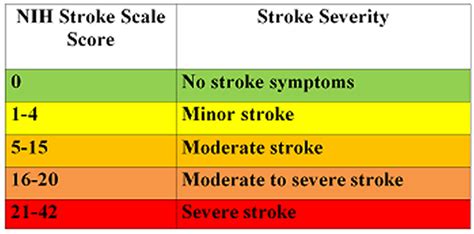
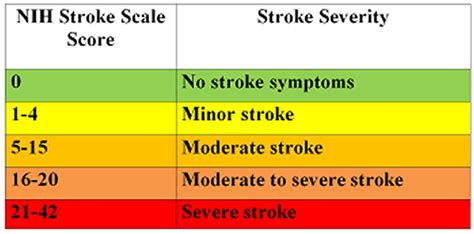
A key aspect of the NIHSS is its role in interpreting stroke severity. This section dives into how the numerical score translates into insights regarding the extent of neurological damage. The scale provides a standardized framework for healthcare professionals to gauge the severity and tailor treatment accordingly.
Mastering the Basics
Mastering the basics of the NIH Stroke Scale is essential for healthcare practitioners. This involves a comprehensive understanding of each component, ensuring accurate assessment and facilitating effective communication among medical teams involved in a patient's care.
Beyond Numbers

Going beyond the numerical figures, the NIHSS score serves as a window into the complexity of strokes. It encapsulates the multifaceted nature of neurological impairment, urging healthcare professionals to view patients holistically and consider the broader implications of their condition.
Conclusion

In conclusion, understanding the key principles of the NIH Stroke Scale score is imperative for healthcare professionals navigating the intricate landscape of stroke assessment. This tool not only aids in immediate decision-making but also contributes to the long-term care and rehabilitation of individuals affected by strokes.
Image sources: Bing Image SearchKey principle to remember about a NIH Stroke Scale score. in Professional's eye
In the realm of healthcare, a nuanced understanding of the
NIH Stroke Scale (NIHSS) score emerges as a cornerstone in the evaluation and management of patients who have experienced a stroke. The
key principle to remember about this assessment tool lies in its meticulous examination of neurological impairments, providing healthcare professionals with a standardized and comprehensive framework to gauge the severity of strokes. As practitioners delve into the intricacies of the NIHSS score, it becomes evident that its application extends far beyond mere numerical representation; it encapsulates a wealth of information crucial for tailored treatment and informed decision-making. This article aims to shed light on the essential principles that underpin the NIHSS score, guiding healthcare practitioners through its significance, practical application, and the intricate balance between standardized evaluation and individualized patient care.
The
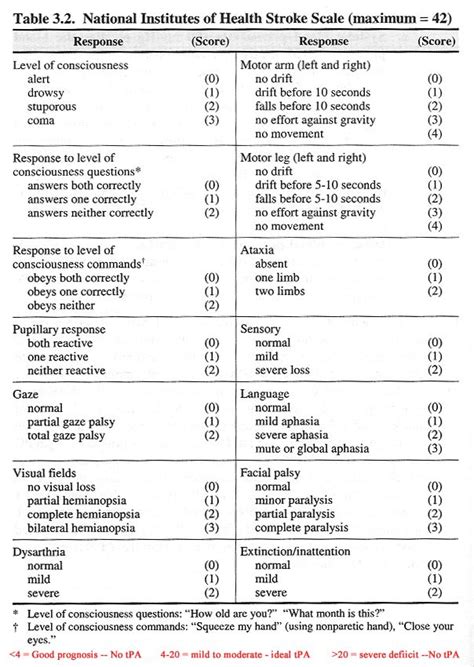
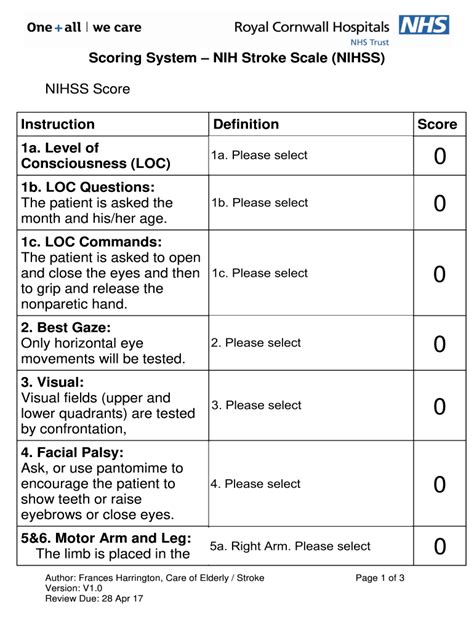
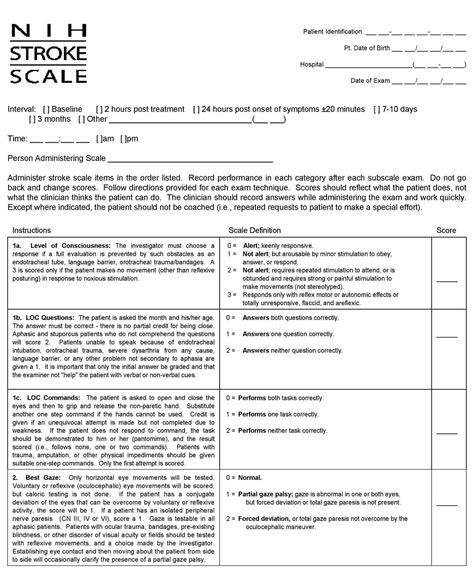
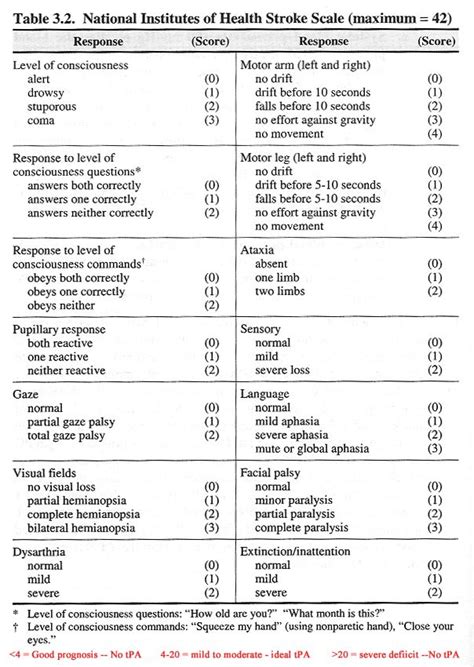
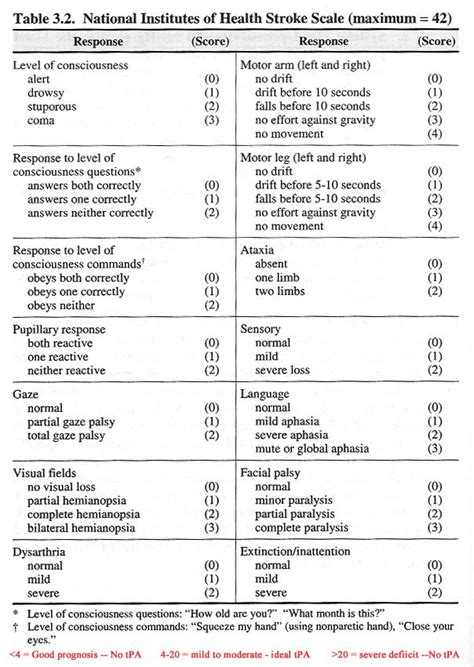
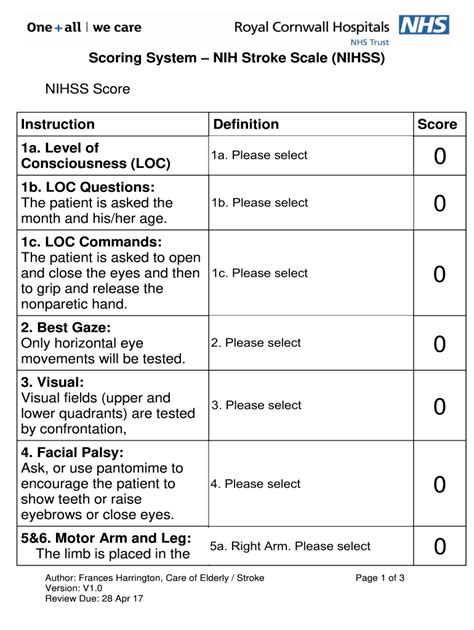
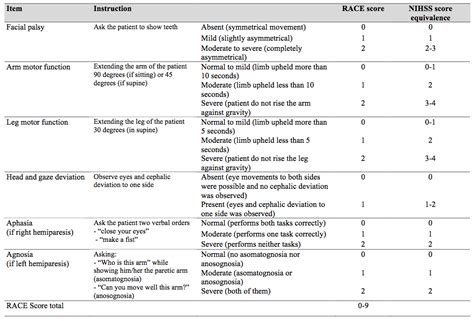
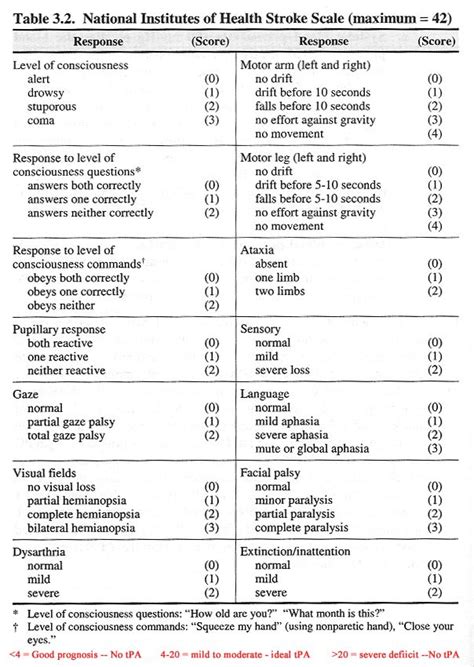
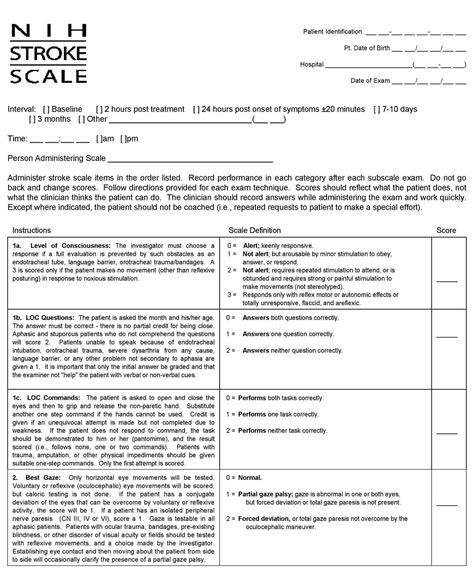
significance of the NIHSS score in stroke assessment cannot be overstated. By comprehensively evaluating motor and sensory functions, language skills, and visual fields, the NIHSS score offers a standardized language for healthcare professionals to communicate the severity of neurological impairments. It serves as a diagnostic compass, guiding practitioners in the initial stages of patient care. Understanding the significance of each component within the scale enables healthcare teams to decipher the complexities of a patient's condition systematically. This standardized approach not only aids in efficient communication among medical professionals but also establishes a foundation for consistent and evidence-based treatment strategies.
Moving beyond theoretical understanding, the
application of the NIHSS score in clinical settings is pivotal for effective patient management. As healthcare practitioners apply the principles of the NIHSS score, they gain actionable insights into the neurological status of patients, facilitating timely interventions. In emergency situations, where rapid and accurate assessments are paramount, the NIHSS score serves as an invaluable tool for triage and decision-making. Its structured approach allows for a systematic examination of neurological deficits, providing a comprehensive overview that guides medical teams in prioritizing interventions and optimizing patient outcomes.

However, despite its undeniable utility, healthcare professionals encounter
challenges in the application of the NIHSS score. Variability in inter-rater reliability, influenced by the experience and training of the assessor, poses a potential hurdle. Additionally, the scale's focus on acute deficits may not fully capture the long-term consequences of stroke, necessitating a comprehensive and multidimensional approach to patient assessment. Overcoming these challenges involves ongoing education and training to enhance the consistency and accuracy of NIHSS score application across diverse clinical settings.
The delicate balance between standardized evaluation and
individualized care remains a crucial consideration in the utilization of the NIHSS score. While the scale provides a systematic framework for assessing stroke severity, healthcare professionals must recognize the unique aspects of each patient's condition. Tailoring interventions based on individual needs requires a holistic understanding that goes beyond the numerical score. This personalized approach involves considering factors such as pre-existing health conditions, patient preferences, and potential long-term consequences, ensuring a comprehensive and patient-centric care plan.
Looking toward the future, ongoing research and
future directions in stroke assessment strive to enhance the precision and applicability of tools like the NIHSS score. Innovations in technology, such as advanced imaging modalities and artificial intelligence, hold promise in refining the accuracy and efficiency of neurological assessments. Additionally, a continued focus on refining scoring methodologies and addressing the limitations of current scales will contribute to a more nuanced understanding of stroke severity and improve outcomes for individuals affected by this debilitating condition.In conclusion, the
NIH Stroke Scale score stands as a pivotal tool in the healthcare landscape, guiding professionals in the assessment and management of strokes. Recognizing the significance of this score, understanding its practical application, acknowledging challenges, embracing individualized care, and remaining attuned to future advancements all contribute to a comprehensive and informed approach to stroke evaluation. As healthcare evolves, so too will the tools at our disposal, ensuring that practitioners can navigate the complexities of stroke care with precision and compassion.
Point of Views : Key principle to remember about a NIH Stroke Scale score.
The
NIH Stroke Scale (NIHSS) score serves as a foundational tool in the assessment of stroke severity within the healthcare domain.Understanding the
key principles embedded in the NIHSS score is imperative for healthcare practitioners engaged in the evaluation and management of stroke patients.This standardized numerical evaluation employs a systematic approach, encompassing various aspects of neurological functioning, including motor skills, sensory perception, language abilities, and visual fields.The
significance of the NIHSS score lies in its ability to provide a common language for healthcare professionals, facilitating consistent communication regarding the severity of neurological impairments observed in stroke patients.Healthcare practitioners rely on the
application of the NIHSS score in clinical settings to make informed decisions swiftly. Its structured methodology aids in triage, ensuring that critical interventions are prioritized based on the severity of neurological deficits.Challenges associated with the NIHSS score, such as variability in inter-rater reliability, underscore the need for ongoing education and training to enhance the accuracy and consistency of its application.Striking a delicate balance between
standardized evaluation and
individualized care, healthcare professionals must recognize the unique aspects of each patient's condition, ensuring that interventions consider personalized factors beyond the numerical score.As healthcare evolves,
future directions in stroke assessment, including advancements in technology and refined scoring methodologies, hold promise in further enhancing the precision and applicability of tools like the NIHSS score.In conclusion, the NIHSS score stands as a crucial instrument, providing a systematic and standardized approach to assess and manage stroke severity. A nuanced understanding of its key principles is essential for healthcare practitioners striving to deliver comprehensive and effective care to stroke patients.
Conclusion :As we draw the curtains on our exploration of the key principles surrounding the NIH Stroke Scale (NIHSS) score, we extend our gratitude for accompanying us on this insightful journey. Unraveling the intricacies of stroke assessment, we have delved into the foundational aspects that make the NIHSS score an indispensable tool in healthcare. From understanding its significance in providing a standardized language for healthcare professionals to its practical application in clinical settings, our exploration has aimed to equip you with a comprehensive understanding of this critical evaluation tool.
As you navigate the healthcare landscape, we encourage you to embrace the individualized care approach, recognizing that the NIHSS score, while a standardized assessment, is a means to a greater end – tailored and compassionate patient care. Looking toward the future, stay attuned to future directions in stroke assessment, as innovations and refinements promise continued advancements in our ability to evaluate and manage stroke severity. We trust that the insights gained from our exploration will not only enhance your understanding of the NIHSS score but also contribute to a holistic perspective on stroke care within the broader healthcare framework. Thank you for being part of our journey in deciphering the key principles of the NIH Stroke Scale score.
Questions and Answer for Key principle to remember about a NIH Stroke Scale score.
Q: What are the key principles to remember about the NIH Stroke Scale score?
- A: The key principles of the NIH Stroke Scale score revolve around its comprehensive evaluation of neurological impairment post-stroke. Understanding the significance of motor skills, sensory perception, language abilities, and visual fields is crucial in interpreting the score accurately.
Q: How is the NIH Stroke Scale score applied in clinical settings?
- A: In clinical settings, the NIH Stroke Scale score is applied as a systematic tool for assessing stroke severity. It aids healthcare professionals in making swift and informed decisions, ensuring that critical interventions are prioritized based on the severity of observed neurological deficits.
Q: What challenges are associated with the NIH Stroke Scale score?
- A: Challenges include variability in inter-rater reliability, emphasizing the need for ongoing education to enhance accuracy. Additionally, the scale's acute focus may not fully capture long-term consequences, prompting a multidimensional approach to patient assessment.
Q: How can healthcare professionals balance standardized evaluation and individualized care with the NIH Stroke Scale score?
- A: Striking a balance involves recognizing the unique aspects of each patient's condition, ensuring that interventions consider personalized factors beyond the numerical score. This approach combines the structured evaluation of the NIHSS score with a holistic and patient-centric care plan.
Q: What does the future hold for stroke assessment and the NIH Stroke Scale score?
- A: Future directions in stroke assessment include technological advancements and refined scoring methodologies. These innovations aim to enhance the precision and applicability of tools like the NIHSS score, contributing to improved outcomes for stroke patients.
Label :NIH Stroke Scale, Healthcare Principles, Stroke Severity, Individualized Care
Keyword : Key principle to remember about a NIH Stroke Scale score.
Explore the essential principles of interpreting NIH Stroke Scale scores. Gain insights crucial for assessing stroke severity, empowering healthcare comprehension.
In the realm of healthcare, a pivotal metric that stands as a linchpin in the assessment of stroke severity is the NIH Stroke Scale (NIHSS) score. Understanding this numerical evaluation is fundamental in deciphering the extent of neurological impairment resulting from a stroke. This article serves as a compass, navigating through the intricate landscape of healthcare topics, with a dedicated focus on unraveling the intricacies of the NIH Stroke Scale score. Delving into the intricacies of its key principles, we aim to equip readers with a comprehensive understanding of this standardized assessment tool. In this pursuit, clarity and objectivity will guide our exploration, avoiding the pitfalls of subjective interpretations. As we embark on this informative journey, it is paramount to recognize the NIH Stroke Scale score as more than a mere numerical figure, but as a critical compass directing healthcare professionals toward a nuanced comprehension of stroke severity.
Top 10 Points about Key principle to remember about a NIH Stroke Scale score. :
- Decoding the NIH Stroke Scale: Unveiling Its Significance
- Understanding Neurological Impairment: A Closer Look at NIHSS Scores
- The Core Principles: Foundation of NIH Stroke Scale Assessment
- Interpreting Stroke Severity: Navigating the NIHSS Landscape
- Crucial Insights: What Every Healthcare Professional Must Grasp
- Key Components of NIHSS: Breaking Down the Assessment
- Why NIH Stroke Scale Matters: Insights into Comprehensive Evaluation
- Mastering the Basics: NIHSS Score as a Fundamental Diagnostic Tool
- Practical Application: Integrating NIH Stroke Scale in Clinical Settings
- Beyond Numbers: NIHSS as a Window into Stroke Complexity
Several facts about Key principle to remember about a NIH Stroke Scale score.
Introduction
Welcome to the intricate world of healthcare, where the NIH Stroke Scale (NIHSS) score emerges as a pivotal tool in understanding and assessing stroke severity. This article endeavors to unravel the key principles that underscore the significance of this numerical evaluation, shedding light on its importance in the realm of neurology.
The Foundation of Assessment
At the core of stroke evaluation lies the NIH Stroke Scale's key principles. Understanding the foundation of this assessment tool is crucial for healthcare professionals tasked with deciphering the neurological impact of strokes. It serves as a comprehensive guide, ensuring a nuanced comprehension of the patient's condition.
Decoding Neurological Impairment
Delving deeper, we uncover the nuances of neurological impairment through the lens of NIHSS scores. Each element of the scale contributes to the holistic understanding of the patient's condition, allowing healthcare practitioners to tailor their approach based on specific impairments identified during the assessment.
Practical Application in Clinical Settings
Bringing theory into practice, the NIH Stroke Scale finds its application in clinical settings. Healthcare professionals utilize this tool to make informed decisions, ensuring that patients receive timely and appropriate interventions based on the severity of their neurological impairment.
Interpreting Stroke Severity
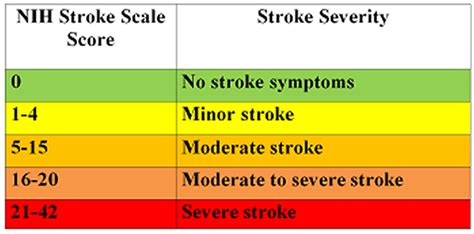
A key aspect of the NIHSS is its role in interpreting stroke severity. This section dives into how the numerical score translates into insights regarding the extent of neurological damage. The scale provides a standardized framework for healthcare professionals to gauge the severity and tailor treatment accordingly.
Mastering the Basics
Mastering the basics of the NIH Stroke Scale is essential for healthcare practitioners. This involves a comprehensive understanding of each component, ensuring accurate assessment and facilitating effective communication among medical teams involved in a patient's care.
Beyond Numbers

Going beyond the numerical figures, the NIHSS score serves as a window into the complexity of strokes. It encapsulates the multifaceted nature of neurological impairment, urging healthcare professionals to view patients holistically and consider the broader implications of their condition.
Conclusion

In conclusion, understanding the key principles of the NIH Stroke Scale score is imperative for healthcare professionals navigating the intricate landscape of stroke assessment. This tool not only aids in immediate decision-making but also contributes to the long-term care and rehabilitation of individuals affected by strokes.
Image sources: Bing Image SearchKey principle to remember about a NIH Stroke Scale score. in Professional's eye
In the realm of healthcare, a nuanced understanding of the
NIH Stroke Scale (NIHSS) score emerges as a cornerstone in the evaluation and management of patients who have experienced a stroke. The
key principle to remember about this assessment tool lies in its meticulous examination of neurological impairments, providing healthcare professionals with a standardized and comprehensive framework to gauge the severity of strokes. As practitioners delve into the intricacies of the NIHSS score, it becomes evident that its application extends far beyond mere numerical representation; it encapsulates a wealth of information crucial for tailored treatment and informed decision-making. This article aims to shed light on the essential principles that underpin the NIHSS score, guiding healthcare practitioners through its significance, practical application, and the intricate balance between standardized evaluation and individualized patient care.
The
significance of the NIHSS score in stroke assessment cannot be overstated. By comprehensively evaluating motor and sensory functions, language skills, and visual fields, the NIHSS score offers a standardized language for healthcare professionals to communicate the severity of neurological impairments. It serves as a diagnostic compass, guiding practitioners in the initial stages of patient care. Understanding the significance of each component within the scale enables healthcare teams to decipher the complexities of a patient's condition systematically. This standardized approach not only aids in efficient communication among medical professionals but also establishes a foundation for consistent and evidence-based treatment strategies.
Moving beyond theoretical understanding, the
application of the NIHSS score in clinical settings is pivotal for effective patient management. As healthcare practitioners apply the principles of the NIHSS score, they gain actionable insights into the neurological status of patients, facilitating timely interventions. In emergency situations, where rapid and accurate assessments are paramount, the NIHSS score serves as an invaluable tool for triage and decision-making. Its structured approach allows for a systematic examination of neurological deficits, providing a comprehensive overview that guides medical teams in prioritizing interventions and optimizing patient outcomes.

However, despite its undeniable utility, healthcare professionals encounter
challenges in the application of the NIHSS score. Variability in inter-rater reliability, influenced by the experience and training of the assessor, poses a potential hurdle. Additionally, the scale's focus on acute deficits may not fully capture the long-term consequences of stroke, necessitating a comprehensive and multidimensional approach to patient assessment. Overcoming these challenges involves ongoing education and training to enhance the consistency and accuracy of NIHSS score application across diverse clinical settings.
The delicate balance between standardized evaluation and
individualized care remains a crucial consideration in the utilization of the NIHSS score. While the scale provides a systematic framework for assessing stroke severity, healthcare professionals must recognize the unique aspects of each patient's condition. Tailoring interventions based on individual needs requires a holistic understanding that goes beyond the numerical score. This personalized approach involves considering factors such as pre-existing health conditions, patient preferences, and potential long-term consequences, ensuring a comprehensive and patient-centric care plan.
Looking toward the future, ongoing research and
future directions in stroke assessment strive to enhance the precision and applicability of tools like the NIHSS score. Innovations in technology, such as advanced imaging modalities and artificial intelligence, hold promise in refining the accuracy and efficiency of neurological assessments. Additionally, a continued focus on refining scoring methodologies and addressing the limitations of current scales will contribute to a more nuanced understanding of stroke severity and improve outcomes for individuals affected by this debilitating condition.In conclusion, the
NIH Stroke Scale score stands as a pivotal tool in the healthcare landscape, guiding professionals in the assessment and management of strokes. Recognizing the significance of this score, understanding its practical application, acknowledging challenges, embracing individualized care, and remaining attuned to future advancements all contribute to a comprehensive and informed approach to stroke evaluation. As healthcare evolves, so too will the tools at our disposal, ensuring that practitioners can navigate the complexities of stroke care with precision and compassion.
Point of Views : Key principle to remember about a NIH Stroke Scale score.
The
NIH Stroke Scale (NIHSS) score serves as a foundational tool in the assessment of stroke severity within the healthcare domain.Understanding the
key principles embedded in the NIHSS score is imperative for healthcare practitioners engaged in the evaluation and management of stroke patients.This standardized numerical evaluation employs a systematic approach, encompassing various aspects of neurological functioning, including motor skills, sensory perception, language abilities, and visual fields.The
significance of the NIHSS score lies in its ability to provide a common language for healthcare professionals, facilitating consistent communication regarding the severity of neurological impairments observed in stroke patients.Healthcare practitioners rely on the
application of the NIHSS score in clinical settings to make informed decisions swiftly. Its structured methodology aids in triage, ensuring that critical interventions are prioritized based on the severity of neurological deficits.Challenges associated with the NIHSS score, such as variability in inter-rater reliability, underscore the need for ongoing education and training to enhance the accuracy and consistency of its application.Striking a delicate balance between
standardized evaluation and
individualized care, healthcare professionals must recognize the unique aspects of each patient's condition, ensuring that interventions consider personalized factors beyond the numerical score.As healthcare evolves,
future directions in stroke assessment, including advancements in technology and refined scoring methodologies, hold promise in further enhancing the precision and applicability of tools like the NIHSS score.In conclusion, the NIHSS score stands as a crucial instrument, providing a systematic and standardized approach to assess and manage stroke severity. A nuanced understanding of its key principles is essential for healthcare practitioners striving to deliver comprehensive and effective care to stroke patients.
Conclusion :As we draw the curtains on our exploration of the key principles surrounding the NIH Stroke Scale (NIHSS) score, we extend our gratitude for accompanying us on this insightful journey. Unraveling the intricacies of stroke assessment, we have delved into the foundational aspects that make the NIHSS score an indispensable tool in healthcare. From understanding its significance in providing a standardized language for healthcare professionals to its practical application in clinical settings, our exploration has aimed to equip you with a comprehensive understanding of this critical evaluation tool.
As you navigate the healthcare landscape, we encourage you to embrace the individualized care approach, recognizing that the NIHSS score, while a standardized assessment, is a means to a greater end – tailored and compassionate patient care. Looking toward the future, stay attuned to future directions in stroke assessment, as innovations and refinements promise continued advancements in our ability to evaluate and manage stroke severity. We trust that the insights gained from our exploration will not only enhance your understanding of the NIHSS score but also contribute to a holistic perspective on stroke care within the broader healthcare framework. Thank you for being part of our journey in deciphering the key principles of the NIH Stroke Scale score.
Questions and Answer for Key principle to remember about a NIH Stroke Scale score.
Q: What are the key principles to remember about the NIH Stroke Scale score?
- A: The key principles of the NIH Stroke Scale score revolve around its comprehensive evaluation of neurological impairment post-stroke. Understanding the significance of motor skills, sensory perception, language abilities, and visual fields is crucial in interpreting the score accurately.
Q: How is the NIH Stroke Scale score applied in clinical settings?
- A: In clinical settings, the NIH Stroke Scale score is applied as a systematic tool for assessing stroke severity. It aids healthcare professionals in making swift and informed decisions, ensuring that critical interventions are prioritized based on the severity of observed neurological deficits.
Q: What challenges are associated with the NIH Stroke Scale score?
- A: Challenges include variability in inter-rater reliability, emphasizing the need for ongoing education to enhance accuracy. Additionally, the scale's acute focus may not fully capture long-term consequences, prompting a multidimensional approach to patient assessment.
Q: How can healthcare professionals balance standardized evaluation and individualized care with the NIH Stroke Scale score?
- A: Striking a balance involves recognizing the unique aspects of each patient's condition, ensuring that interventions consider personalized factors beyond the numerical score. This approach combines the structured evaluation of the NIHSS score with a holistic and patient-centric care plan.
Q: What does the future hold for stroke assessment and the NIH Stroke Scale score?
- A: Future directions in stroke assessment include technological advancements and refined scoring methodologies. These innovations aim to enhance the precision and applicability of tools like the NIHSS score, contributing to improved outcomes for stroke patients.
Label :NIH Stroke Scale, Healthcare Principles, Stroke Severity, Individualized Care
Keyword : Key principle to remember about a NIH Stroke Scale score.
0 komentar