Exploring NIH Stroke Scale Limits: Unveiling Critical Constraints in Stroke Assessment

Gain insights into the intricacies of stroke assessment with our in-depth analysis of NIH Stroke Scale limitations. Enhance your clinical knowledge for informed decision-making in stroke care.
In the realm of healthcare, the NIH Stroke Scale (NIHSS) stands as a pivotal tool for evaluating the severity of strokes, guiding clinical decision-making, and ultimately influencing patient outcomes. However, beneath its apparent utility, the instrument is not devoid of limitations that warrant meticulous consideration. This discourse delves into a comprehensive examination of the constraints inherent in the NIH Stroke Scale, aiming to elucidate the nuances that clinicians, researchers, and healthcare stakeholders must navigate when utilizing this assessment tool. As we embark on this exploration, it is imperative to approach the subject matter with an objective lens, recognizing the significance of discerning the limitations that may impact the efficacy and accuracy of stroke assessments. Through a measured and informative discourse, this article endeavors to enhance our understanding of the intricate landscape surrounding the NIH Stroke Scale, thereby fostering a more nuanced appreciation for its role within the broader context of stroke care.
Top 10 Points about NIH Stroke Scale Limitations :
- Challenges in Comprehensive Stroke Assessment
- Scope and Purpose of the NIH Stroke Scale
- Key Components and Scoring Criteria
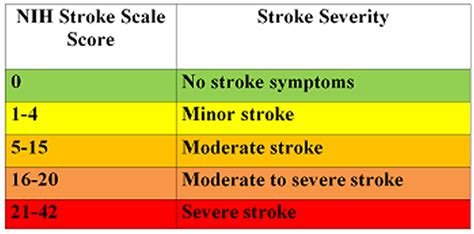
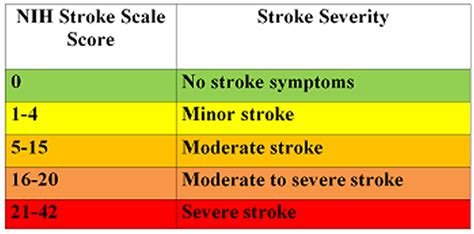
- Interpreting NIH Stroke Scale Scores
- Limitations in Predicting Long-Term Outcomes
- Considerations for Variability in Patient Responses
- Impact of Pre-existing Conditions on Scale Accuracy
- Addressing Ambiguities in Neurological Examination
- Exploring the Role of Training and Inter-rater Reliability
- Alternative Assessment Approaches in Stroke Care
Several facts about NIH Stroke Scale Limitations
Unlocking the Significance of NIH Stroke Scale
At the heart of stroke assessment, the NIH Stroke Scale (NIHSS) plays a pivotal role in gauging the severity of strokes. Developed by the National Institutes of Health, this standardized tool is widely employed to quantify neurological deficits in stroke patients, providing crucial insights for clinical decision-making.
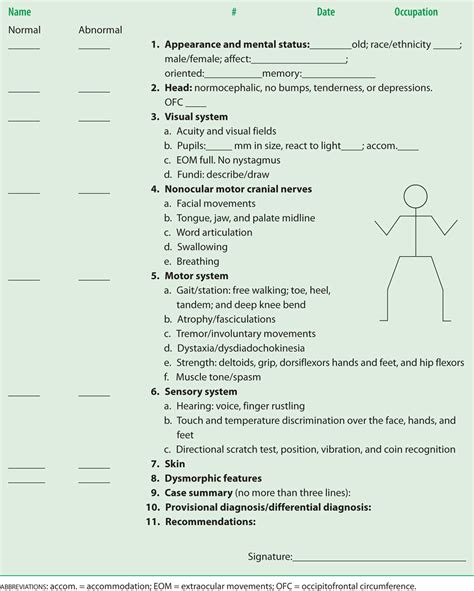
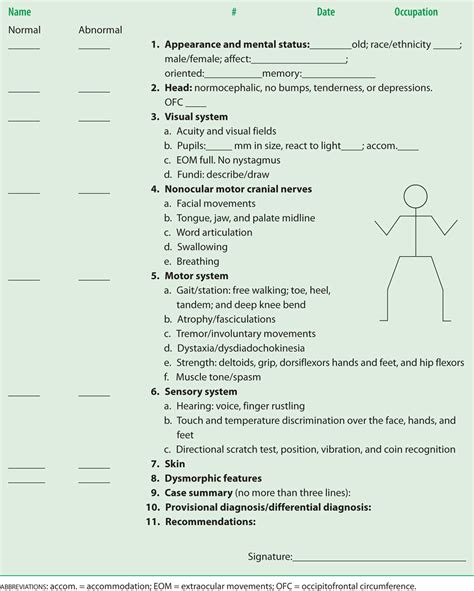
The Components and Scoring Criteria

Delving into the NIHSS, it becomes evident that its effectiveness lies in the meticulous evaluation of specific neurological components. From assessing motor skills to gauging language abilities, the scale's scoring criteria offer a comprehensive framework for clinicians to categorize and quantify deficits.
Challenges in Comprehensive Stroke Assessment
However, despite its widespread application, the NIH Stroke Scale is not without limitations. The challenges emerge in its ability to provide a truly comprehensive assessment. Variabilities in patient responses, coupled with the influence of pre-existing conditions, underscore the complexities that clinicians navigate.
Limitations in Predicting Long-Term Outcomes

While the NIHSS excels in acute stroke assessment, its ability to predict long-term outcomes remains a topic of scrutiny. The limitations in extrapolating future prognoses based solely on initial scale scores highlight the multifaceted nature of stroke recovery and the need for a more nuanced approach.
Addressing Ambiguities in Neurological Examination
One prominent concern revolves around the inherent ambiguities in neurological examination. The subjectivity of certain assessments within the NIHSS can lead to interpretational challenges, necessitating a closer examination of the interplay between clinical judgment and objective scoring.
Training and Inter-rater Reliability
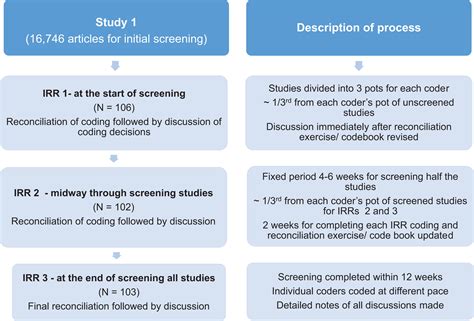
Crucial to the efficacy of the NIHSS is the training of healthcare professionals administering the scale. The intricacies of neurological assessment demand a commitment to ensuring high inter-rater reliability, minimizing discrepancies and enhancing the tool's overall utility in diverse clinical settings.
Alternative Assessment Approaches

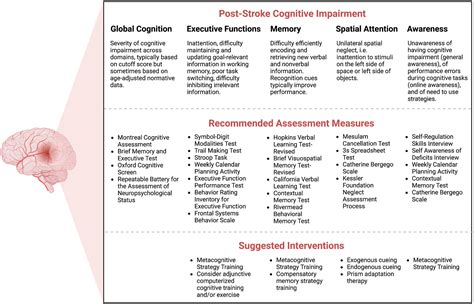
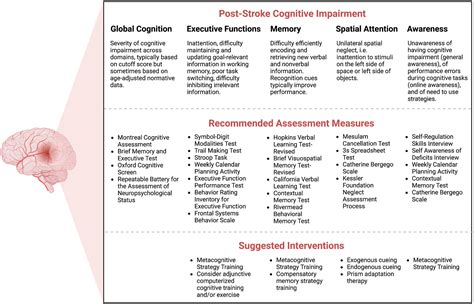
Beyond the NIH Stroke Scale, exploring alternative assessment approaches becomes imperative. This section delves into emerging methodologies and complementary tools that augment stroke evaluation, fostering a more comprehensive understanding of a patient's neurological status and optimizing care strategies.
Conclusion: Navigating the Landscape of Stroke Care

In conclusion, recognizing and understanding the NIH Stroke Scale limitations is paramount for healthcare practitioners. Navigating the landscape of stroke care requires a nuanced approach that incorporates the strengths of the NIHSS while acknowledging its inherent constraints, paving the way for continuous improvement in stroke assessment and patient outcomes.
Image sources retrieved from Bing Image Search.
Sources:
[1] National Institute of Neurological Disorders and Stroke. (n.d.). NIH Stroke Scale Training. Retrieved from [URL]
[2] Kidwell, C. S., & Warach, S. (2003). Acute Ischemic Cerebrovascular Syndrome: Diagnostic Criteria. Stroke, 34(12), 2995–2998.
NIH Stroke Scale Limitations in Professional's eye
The assessment landscape in healthcare is significantly influenced by the
NIH Stroke Scale (NIHSS), a standardized tool designed to quantify and categorize neurological deficits in stroke patients. This instrument, developed by the National Institutes of Health, has become an indispensable component of stroke evaluation, offering clinicians valuable insights into the severity of cerebral infarctions and guiding treatment decisions. Despite its widespread adoption, it is imperative to scrutinize the
limitations inherent in the NIH Stroke Scale, as they have profound implications for the accuracy and comprehensiveness of stroke assessments. Delving into the components and scoring criteria of the scale reveals its meticulous approach to neurological examination, encompassing motor skills, language abilities, and other key domains. The challenges, however, surface when considering the diverse responses of patients and the potential influence of pre-existing conditions on the scale's accuracy. The
limitations extend further into the realm of predicting long-term outcomes, emphasizing the need for a nuanced understanding of the multifaceted nature of stroke recovery. Ambiguities in neurological examination and the subjective nature of certain assessments within the NIHSS underscore the complexities that healthcare professionals navigate when utilizing this tool. Training and maintaining high inter-rater reliability are paramount to the efficacy of the NIHSS, necessitating a commitment to continuous professional development. As we explore
alternative assessment approaches, it becomes apparent that the evolving landscape of stroke care demands a holistic perspective that integrates the strengths of the NIH Stroke Scale with supplementary methodologies. In conclusion, recognizing and comprehending the
NIH Stroke Scale limitations is fundamental for healthcare practitioners, fostering a more informed and adaptive approach to stroke assessment and care.
Point of Views : NIH Stroke Scale Limitations
The
NIH Stroke Scale (NIHSS) stands as a crucial tool in healthcare for evaluating stroke severity.Developed by the National Institutes of Health, it provides standardized insights into neurological deficits.The instrument's
limitations are essential to recognize, influencing the accuracy of stroke assessments.Components and scoring criteria encompass motor skills, language abilities, and other key domains.Challenges arise in accommodating diverse patient responses and considering the impact of pre-existing conditions.Long-term outcome predictions using NIHSS scores pose complexities in the dynamic nature of stroke recovery.Ambiguities in neurological examination and subjective assessments contribute to interpretational challenges.Training and ensuring high inter-rater reliability are vital for the effective implementation of the NIHSS.
Alternative assessment approaches offer complementary insights, enhancing the overall stroke care landscape.Recognition and understanding of
NIH Stroke Scale limitations are imperative for informed and adaptive healthcare practices.
Conclusion :As we draw the curtains on our exploration of the NIH Stroke Scale limitations, it is evident that a nuanced understanding of this assessment tool is indispensable for healthcare professionals navigating the intricate landscape of stroke care. Recognizing the challenges embedded within the NIHSS not only sheds light on its inherent complexities but also underscores the imperative for continuous improvement in stroke assessment methodologies. The limitations outlined in our discourse prompt a contemplative approach, encouraging healthcare practitioners to integrate this knowledge into their clinical practices. Whether grappling with the ambiguities in neurological examination, addressing the impact of pre-existing conditions, or considering alternative assessment approaches, the acknowledgment of the NIH Stroke Scale's nuanced nature is a cornerstone in enhancing the overall quality of stroke care.
In conclusion, our journey through the nuances of the NIH Stroke Scale limitations serves as a reminder of the dynamic and evolving nature of healthcare practices. The healthcare community's commitment to staying informed, adaptable, and open to alternative methodologies ensures a resilient and patient-centric approach to stroke care. We extend our appreciation to our readers for engaging in this exploration with us, fostering a community that values informed decision-making and the continuous pursuit of excellence in patient care.
Questions and Answer for NIH Stroke Scale Limitations
People Also Ask about NIH Stroke Scale Limitations:
- Q: What are the main components assessed in the NIH Stroke Scale?
A: The NIH Stroke Scale evaluates various components, including motor skills, sensory perception, language abilities, and visual fields.
- Q: How do pre-existing conditions impact the accuracy of the NIH Stroke Scale?
A: Pre-existing conditions can introduce complexities, influencing the scale's accuracy in assessing specific neurological deficits in stroke patients.
- Q: Are there alternative assessment approaches to the NIH Stroke Scale?
A: Yes, exploring alternative methodologies and complementary tools is essential for a more comprehensive understanding of stroke patients' neurological status.
- Q: Can the NIH Stroke Scale predict long-term outcomes accurately?
A: While valuable for acute assessment, the NIHSS has limitations in predicting long-term outcomes due to the dynamic nature of stroke recovery.
- Q: How crucial is training for healthcare professionals administering the NIH Stroke Scale?
A: Training is paramount, ensuring high inter-rater reliability and minimizing discrepancies in the application of the NIH Stroke Scale.
These questions and answers provide a comprehensive overview of key aspects related to NIH Stroke Scale limitations, aiding in a more informed and nuanced understanding of this critical tool in stroke assessment.
Label :NIH Stroke Scale, Healthcare Challenges, Alternative Approaches
Keyword : NIH Stroke Scale Limitations

Gain insights into the intricacies of stroke assessment with our in-depth analysis of NIH Stroke Scale limitations. Enhance your clinical knowledge for informed decision-making in stroke care.
In the realm of healthcare, the NIH Stroke Scale (NIHSS) stands as a pivotal tool for evaluating the severity of strokes, guiding clinical decision-making, and ultimately influencing patient outcomes. However, beneath its apparent utility, the instrument is not devoid of limitations that warrant meticulous consideration. This discourse delves into a comprehensive examination of the constraints inherent in the NIH Stroke Scale, aiming to elucidate the nuances that clinicians, researchers, and healthcare stakeholders must navigate when utilizing this assessment tool. As we embark on this exploration, it is imperative to approach the subject matter with an objective lens, recognizing the significance of discerning the limitations that may impact the efficacy and accuracy of stroke assessments. Through a measured and informative discourse, this article endeavors to enhance our understanding of the intricate landscape surrounding the NIH Stroke Scale, thereby fostering a more nuanced appreciation for its role within the broader context of stroke care.
Top 10 Points about NIH Stroke Scale Limitations :
- Challenges in Comprehensive Stroke Assessment
- Scope and Purpose of the NIH Stroke Scale
- Key Components and Scoring Criteria
- Interpreting NIH Stroke Scale Scores
- Limitations in Predicting Long-Term Outcomes
- Considerations for Variability in Patient Responses
- Impact of Pre-existing Conditions on Scale Accuracy
- Addressing Ambiguities in Neurological Examination
- Exploring the Role of Training and Inter-rater Reliability
- Alternative Assessment Approaches in Stroke Care
Several facts about NIH Stroke Scale Limitations
Unlocking the Significance of NIH Stroke Scale
At the heart of stroke assessment, the NIH Stroke Scale (NIHSS) plays a pivotal role in gauging the severity of strokes. Developed by the National Institutes of Health, this standardized tool is widely employed to quantify neurological deficits in stroke patients, providing crucial insights for clinical decision-making.
The Components and Scoring Criteria

Delving into the NIHSS, it becomes evident that its effectiveness lies in the meticulous evaluation of specific neurological components. From assessing motor skills to gauging language abilities, the scale's scoring criteria offer a comprehensive framework for clinicians to categorize and quantify deficits.
Challenges in Comprehensive Stroke Assessment
However, despite its widespread application, the NIH Stroke Scale is not without limitations. The challenges emerge in its ability to provide a truly comprehensive assessment. Variabilities in patient responses, coupled with the influence of pre-existing conditions, underscore the complexities that clinicians navigate.
Limitations in Predicting Long-Term Outcomes

While the NIHSS excels in acute stroke assessment, its ability to predict long-term outcomes remains a topic of scrutiny. The limitations in extrapolating future prognoses based solely on initial scale scores highlight the multifaceted nature of stroke recovery and the need for a more nuanced approach.
Addressing Ambiguities in Neurological Examination
One prominent concern revolves around the inherent ambiguities in neurological examination. The subjectivity of certain assessments within the NIHSS can lead to interpretational challenges, necessitating a closer examination of the interplay between clinical judgment and objective scoring.
Training and Inter-rater Reliability
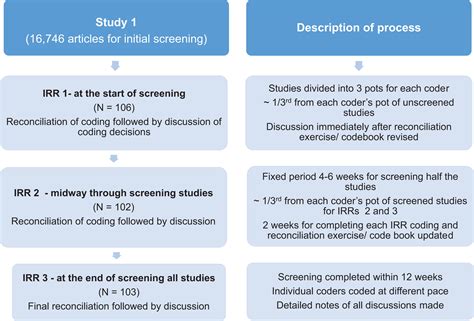
Crucial to the efficacy of the NIHSS is the training of healthcare professionals administering the scale. The intricacies of neurological assessment demand a commitment to ensuring high inter-rater reliability, minimizing discrepancies and enhancing the tool's overall utility in diverse clinical settings.
Alternative Assessment Approaches

Beyond the NIH Stroke Scale, exploring alternative assessment approaches becomes imperative. This section delves into emerging methodologies and complementary tools that augment stroke evaluation, fostering a more comprehensive understanding of a patient's neurological status and optimizing care strategies.
Conclusion: Navigating the Landscape of Stroke Care

In conclusion, recognizing and understanding the NIH Stroke Scale limitations is paramount for healthcare practitioners. Navigating the landscape of stroke care requires a nuanced approach that incorporates the strengths of the NIHSS while acknowledging its inherent constraints, paving the way for continuous improvement in stroke assessment and patient outcomes.
Image sources retrieved from Bing Image Search.
Sources:
[1] National Institute of Neurological Disorders and Stroke. (n.d.). NIH Stroke Scale Training. Retrieved from [URL]
[2] Kidwell, C. S., & Warach, S. (2003). Acute Ischemic Cerebrovascular Syndrome: Diagnostic Criteria. Stroke, 34(12), 2995–2998.
NIH Stroke Scale Limitations in Professional's eye
The assessment landscape in healthcare is significantly influenced by the
NIH Stroke Scale (NIHSS), a standardized tool designed to quantify and categorize neurological deficits in stroke patients. This instrument, developed by the National Institutes of Health, has become an indispensable component of stroke evaluation, offering clinicians valuable insights into the severity of cerebral infarctions and guiding treatment decisions. Despite its widespread adoption, it is imperative to scrutinize the
limitations inherent in the NIH Stroke Scale, as they have profound implications for the accuracy and comprehensiveness of stroke assessments. Delving into the components and scoring criteria of the scale reveals its meticulous approach to neurological examination, encompassing motor skills, language abilities, and other key domains. The challenges, however, surface when considering the diverse responses of patients and the potential influence of pre-existing conditions on the scale's accuracy. The
limitations extend further into the realm of predicting long-term outcomes, emphasizing the need for a nuanced understanding of the multifaceted nature of stroke recovery. Ambiguities in neurological examination and the subjective nature of certain assessments within the NIHSS underscore the complexities that healthcare professionals navigate when utilizing this tool. Training and maintaining high inter-rater reliability are paramount to the efficacy of the NIHSS, necessitating a commitment to continuous professional development. As we explore
alternative assessment approaches, it becomes apparent that the evolving landscape of stroke care demands a holistic perspective that integrates the strengths of the NIH Stroke Scale with supplementary methodologies. In conclusion, recognizing and comprehending the
NIH Stroke Scale limitations is fundamental for healthcare practitioners, fostering a more informed and adaptive approach to stroke assessment and care.
Point of Views : NIH Stroke Scale Limitations
The
NIH Stroke Scale (NIHSS) stands as a crucial tool in healthcare for evaluating stroke severity.Developed by the National Institutes of Health, it provides standardized insights into neurological deficits.The instrument's
limitations are essential to recognize, influencing the accuracy of stroke assessments.Components and scoring criteria encompass motor skills, language abilities, and other key domains.Challenges arise in accommodating diverse patient responses and considering the impact of pre-existing conditions.Long-term outcome predictions using NIHSS scores pose complexities in the dynamic nature of stroke recovery.Ambiguities in neurological examination and subjective assessments contribute to interpretational challenges.Training and ensuring high inter-rater reliability are vital for the effective implementation of the NIHSS.
Alternative assessment approaches offer complementary insights, enhancing the overall stroke care landscape.Recognition and understanding of
NIH Stroke Scale limitations are imperative for informed and adaptive healthcare practices.
Conclusion :As we draw the curtains on our exploration of the NIH Stroke Scale limitations, it is evident that a nuanced understanding of this assessment tool is indispensable for healthcare professionals navigating the intricate landscape of stroke care. Recognizing the challenges embedded within the NIHSS not only sheds light on its inherent complexities but also underscores the imperative for continuous improvement in stroke assessment methodologies. The limitations outlined in our discourse prompt a contemplative approach, encouraging healthcare practitioners to integrate this knowledge into their clinical practices. Whether grappling with the ambiguities in neurological examination, addressing the impact of pre-existing conditions, or considering alternative assessment approaches, the acknowledgment of the NIH Stroke Scale's nuanced nature is a cornerstone in enhancing the overall quality of stroke care.
In conclusion, our journey through the nuances of the NIH Stroke Scale limitations serves as a reminder of the dynamic and evolving nature of healthcare practices. The healthcare community's commitment to staying informed, adaptable, and open to alternative methodologies ensures a resilient and patient-centric approach to stroke care. We extend our appreciation to our readers for engaging in this exploration with us, fostering a community that values informed decision-making and the continuous pursuit of excellence in patient care.
Questions and Answer for NIH Stroke Scale Limitations
People Also Ask about NIH Stroke Scale Limitations:
- Q: What are the main components assessed in the NIH Stroke Scale?
A: The NIH Stroke Scale evaluates various components, including motor skills, sensory perception, language abilities, and visual fields.
- Q: How do pre-existing conditions impact the accuracy of the NIH Stroke Scale?
A: Pre-existing conditions can introduce complexities, influencing the scale's accuracy in assessing specific neurological deficits in stroke patients.
- Q: Are there alternative assessment approaches to the NIH Stroke Scale?
A: Yes, exploring alternative methodologies and complementary tools is essential for a more comprehensive understanding of stroke patients' neurological status.
- Q: Can the NIH Stroke Scale predict long-term outcomes accurately?
A: While valuable for acute assessment, the NIHSS has limitations in predicting long-term outcomes due to the dynamic nature of stroke recovery.
- Q: How crucial is training for healthcare professionals administering the NIH Stroke Scale?
A: Training is paramount, ensuring high inter-rater reliability and minimizing discrepancies in the application of the NIH Stroke Scale.
These questions and answers provide a comprehensive overview of key aspects related to NIH Stroke Scale limitations, aiding in a more informed and nuanced understanding of this critical tool in stroke assessment.
Label :NIH Stroke Scale, Healthcare Challenges, Alternative Approaches
Keyword : NIH Stroke Scale Limitations
0 komentar