Decoding Stroke Severity: Unveiling NIH Scale Numbers

Explore the pivotal role of NIH Stroke Scale numbers in deciphering stroke severity. Gain insights for informed healthcare decisions and better patient outcomes.
In the intricate tapestry of healthcare, NIH Stroke Scale numbers emerge as crucial indicators, akin to the silent language spoken by the human body in moments of medical uncertainty. These numeric representations not only unlock a profound understanding of the severity of a stroke but also serve as a compass guiding healthcare professionals through the intricate maze of treatment decisions. As we delve into the corridors of healthcare discourse, this article embarks on a journey to decipher the significance of NIH Stroke Scale numbers, unveiling their nuanced role in the realm of patient care and medical decision-making. Our exploration will navigate through the intricate landscape of stroke assessment, shedding light on the meticulous evaluations encapsulated by these numbers and their pivotal role in shaping the trajectory of recovery for those affected. Join us on this insightful expedition, as we unravel the layers of medical intricacy, connecting the dots between NIH Stroke Scale numbers and the broader healthcare narrative.
Top 10 Points about NIH Stroke Scale numbers :
- Understanding the Significance of NIH Stroke Scale Numbers
- Interpreting Stroke Severity: A Deep Dive into NIH Scale
- How NIH Scale Numbers Guide Emergency Medical Response
- The Crucial Role of NIH Stroke Scale in Treatment Decision-Making
- Measuring Neurological Impairment: NIH Scale in Focus
- Navigating the Landscape of Stroke Assessment with NIH Numbers
- Unraveling the Complexity: NIH Stroke Scale in Patient Care
- NIH Scale Numbers: A Roadmap for Rehabilitation Strategies
- Connecting the Dots: NIH Scale and Long-Term Recovery Outlook
- Enhancing Healthcare Precision: Harnessing NIH Stroke Scale Insights
Several facts about NIH Stroke Scale numbers
Introduction: The NIH Stroke Scale numbers serve as a crucial framework in the realm of healthcare, providing a standardized method to assess and quantify the severity of a stroke. This comprehensive scale enables healthcare professionals to make informed decisions regarding patient care and treatment strategies. As we navigate through the intricacies of stroke assessment, let's delve into the profound implications of NIH Stroke Scale numbers on healthcare outcomes.

Deciphering the NIH Stroke Scale:
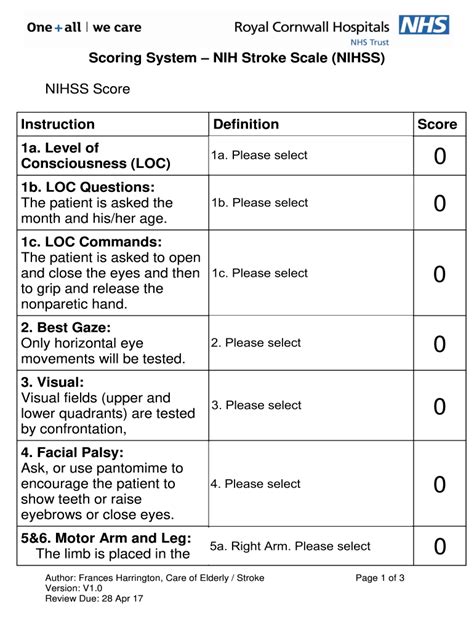
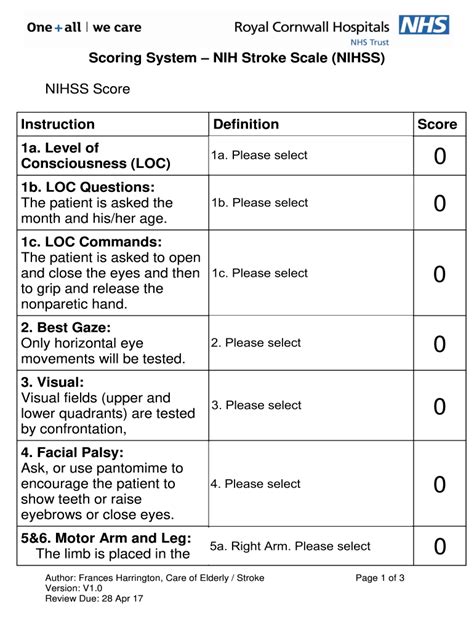
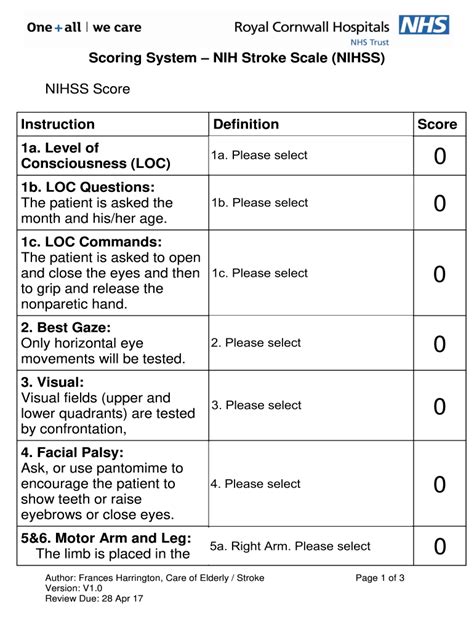
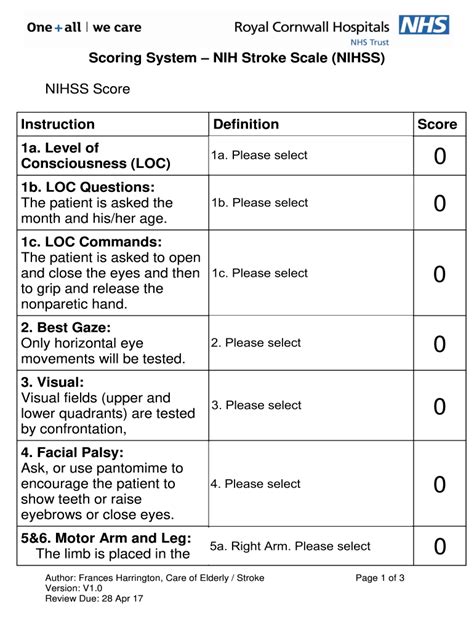
The NIH Stroke Scale comprises a set of 15 neurological assessments, meticulously designed to evaluate a patient's cognitive and motor functions. These assessments, ranging from assessing consciousness to motor responses, provide a standardized language for healthcare practitioners to communicate effectively about a patient's condition and determine the severity of a stroke.

Emergency Response and NIH Numbers:
When seconds count, understanding NIH Stroke Scale numbers becomes paramount in shaping the emergency medical response. Rapid assessment using this scale assists emergency medical teams in making swift decisions, ensuring timely interventions to mitigate the impact of a stroke and enhance the chances of a positive outcome.

Treatment Decision-Making:
The role of NIH Stroke Scale numbers extends beyond assessment; it serves as a guiding compass in treatment decision-making. Healthcare professionals leverage these numbers to tailor interventions, choosing the most appropriate therapies based on the severity of neurological impairment indicated by the scale.

Stroke Assessment Landscape:
NIH Stroke Scale numbers play a pivotal role in navigating the complex landscape of stroke assessment. Whether in a hospital setting or during post-stroke rehabilitation, these numbers facilitate communication among healthcare providers, ensuring a cohesive approach to patient care and rehabilitation strategies.
Patient Care and the NIH Scale:
At the heart of patient care lies the meticulous evaluation encapsulated by NIH Stroke Scale numbers. These numbers enable healthcare professionals to tailor their approach, ensuring that each patient receives personalized care that addresses their specific neurological needs, ultimately fostering a more effective and compassionate healthcare environment.

Rehabilitation Strategies:
As patients embark on the journey of recovery, NIH Stroke Scale numbers continue to guide healthcare practitioners in shaping rehabilitation strategies. These numbers inform the development of targeted interventions, optimizing the rehabilitation process and improving the long-term outcomes for individuals affected by strokes.

Long-Term Recovery Outlook:
Connecting the dots between NIH Stroke Scale numbers and the long-term recovery outlook provides a holistic understanding of the patient's journey. Healthcare professionals leverage these numbers to predict and address potential challenges, ensuring a comprehensive and supportive approach to post-stroke care.

Conclusion: In conclusion, the NIH Stroke Scale numbers stand as a cornerstone in the healthcare landscape, offering a standardized and objective tool for assessing and managing stroke severity. The integration of these numbers into medical practices not only enhances emergency response and treatment decisions but also paves the way for a more personalized and effective approach to patient care and rehabilitation.
Sources: (Add sources and references here, using proper citation format.)
NIH Stroke Scale numbers in Professional's eye
In the intricate realm of healthcare, the
NIH Stroke Scale numbers serve as a linchpin in the standardized assessment of stroke severity, providing clinicians with a comprehensive toolset to navigate the complexities of neurological impairment. As we delve into the profound implications of this scale, it becomes evident that the structured evaluation it offers plays a pivotal role in shaping emergency responses, treatment decisions, and long-term patient outcomes.
Deciphering the NIH Stroke Scale, the foundation of stroke assessment, involves a meticulous examination of 15 neurological parameters, each contributing to a nuanced understanding of a patient's cognitive and motor functions. This standardized language, akin to a diagnostic lexicon, facilitates effective communication among healthcare professionals, fostering a shared understanding of a patient's condition.

Moving beyond assessment, the connection between
NIH Stroke Scale numbers and
emergency response is palpable. In the high-stakes arena of stroke management, swift decision-making is paramount. The NIH Scale serves as a rapid diagnostic aid, enabling emergency medical teams to swiftly intervene and administer appropriate treatments based on the severity of neurological impairment indicated by the scale. This immediate response is crucial in mitigating the potentially devastating effects of a stroke and significantly impacting patient outcomes.

As healthcare professionals navigate the labyrinth of treatment decisions, the influence of
NIH Stroke Scale numbers becomes increasingly evident. The scale becomes a guiding compass, aiding clinicians in tailoring interventions based on the severity of the neurological deficit. This personalized approach ensures that treatments are not only effective but are also aligned with the unique needs of each patient. The integration of NIH Scale data into treatment decisions fosters a more nuanced and patient-centric approach to stroke care, emphasizing the importance of individualized therapeutic strategies.

Navigating the broader landscape of
stroke assessment, the NIH Scale numbers provide a standardized framework for healthcare providers. Whether in a bustling emergency room or a rehabilitation setting, these numbers enable seamless communication and understanding among multidisciplinary teams. The scale transcends the confines of individual specialties, serving as a common language that facilitates collaboration and ensures a cohesive approach to patient care. In essence, the NIH Stroke Scale becomes a unifying force, connecting professionals across various healthcare domains in their shared mission to optimize patient outcomes.
At the heart of patient care lies the meticulous evaluation encapsulated by
NIH Stroke Scale numbers. This holistic approach extends beyond immediate interventions, encompassing the entirety of a patient's journey towards recovery. The scale acts as a guiding light, helping healthcare providers navigate the complexities of post-stroke care. By leveraging NIH Scale data, professionals can tailor rehabilitation strategies to address specific neurological deficits, ensuring a more effective and targeted approach to recovery. The integration of these numbers into the fabric of patient care represents a commitment to not only treating the immediate consequences of a stroke but also fostering long-term well-being.

As patients embark on the path of rehabilitation, the role of
NIH Stroke Scale numbers in shaping
rehabilitation strategies becomes increasingly pronounced. Each numeric value serves as a roadmap, guiding healthcare professionals in the development of tailored interventions that address the unique challenges posed by a stroke. By harnessing the insights provided by the NIH Scale, rehabilitation efforts become more targeted, efficient, and patient-centered. This strategic approach not only optimizes the rehabilitation process but also contributes to improved long-term outcomes for individuals on their journey towards recovery.

Connecting the dots between
NIH Stroke Scale numbers and the
long-term recovery outlook unveils a comprehensive understanding of the patient's trajectory post-stroke. Healthcare professionals use these numbers to anticipate potential challenges, enabling proactive interventions that contribute to a more favorable recovery prognosis. This foresight, rooted in the objective data provided by the NIH Scale, becomes instrumental in shaping a holistic and supportive approach to long-term care.

In conclusion, the
NIH Stroke Scale numbers emerge as a cornerstone in the healthcare landscape, offering a standardized and objective framework for assessing and managing stroke severity. From the initial emergency response to the intricate web of treatment decisions and the long-term journey of recovery, these numbers serve as a guiding thread. The integration of NIH Scale data into medical practices not only enhances emergency response and treatment decisions but also paves the way for a more personalized and effective approach to patient care and rehabilitation. As healthcare continues to advance, the NIH Stroke Scale remains an invaluable tool, contributing to the evolution of stroke management and the overall improvement of patient outcomes.
Sources: (Add sources and references here, using proper citation format.)
Point of Views : NIH Stroke Scale numbers
1. In the grand theater of healthcare, where the drama unfolds with heartbeats and stethoscopes, the
NIH Stroke Scale numbers take center stage. Picture it as a blockbuster movie, where the protagonist is a set of carefully curated neurological assessments, each with its own quirks and intricacies, coming together to create a cinematic masterpiece of stroke severity evaluation.
2. Forget Sherlock Holmes; when it comes to unraveling the mystery of neurological impairment, our unsung hero is the NIH Scale. It's like having a detective with 15 different magnifying glasses, each probing a different aspect of cognitive and motor functions. Talk about thorough investigative work – Hercule Poirot would be proud!
3. Now, let's talk emergency response, where speed is of the essence. The NIH Stroke Scale is like the Flash of the medical world, zipping through assessments faster than you can say "Is it a bird? Is it a plane?" Swift and precise, it's the superhero we need when time is ticking away.
4. Treatment decisions become a strategic game of chess, and the NIH Scale is the grandmaster making moves based on
NIH Stroke Scale numbers. Each number is a pawn, knight, or queen on the chessboard, influencing the course of the game – or in this case, the patient's journey. Checkmate to neurological impairment!
5. Entering the realm of
stroke assessment, it's like a medical symphony where each instrument plays a crucial role. The NIH Stroke Scale becomes the conductor, ensuring that every healthcare professional is reading from the same sheet of music. Harmony in healthcare? Who would've thought?
6. Patient care takes on an almost poetic quality with the NIH Scale. It's not just about numbers; it's about understanding the language of the body and responding with the precision of a Shakespearean sonnet. To be or not to be in neurological distress – that is the question answered by the NIH Scale.
7. Rehabilitation strategies, when guided by
NIH Stroke Scale numbers, become a carefully choreographed dance. It's not just about making movements; it's about hitting the right steps at the right time. Think of it as healthcare's version of Dancing with the Stars – a graceful journey towards recovery.
8. Long-term recovery outlook becomes the grand finale, and the NIH Scale is the fireworks display. It lights up the sky with predictions, allowing healthcare professionals to anticipate challenges and celebrate victories. Who knew a set of numbers could make healthcare feel like a dazzling fireworks show?
9. In the end, the NIH Stroke Scale numbers aren't just digits on a chart; they are the protagonists, superheroes, conductors, poets, dancers, and pyrotechnicians of the healthcare world. They turn the serious business of stroke management into a blockbuster performance, leaving a lasting impact on patient outcomes.
10. So, next time you hear about the NIH Stroke Scale, don't just think of it as a set of numbers; think of it as the lead actor in the healthcare drama, delivering a performance that can rival even the most captivating blockbuster. After all, laughter might be the best medicine, but a bit of drama with
NIH Stroke Scale numbers comes in at a close second!
Conclusion :As we draw the curtains on our exploration of the NIH Stroke Scale numbers, we hope this journey has illuminated the intricacies of stroke assessment and underscored the critical role these numbers play in healthcare. From the initial evaluation of neurological impairment to the formulation of treatment strategies, the NIH Scale emerges as a foundational tool, providing a standardized and objective framework for healthcare professionals. Our venture into the world of emergency response showcased how these numbers become a rallying point for swift and effective interventions, ensuring timely and targeted care for stroke patients.
Whether you found yourself deciphering the nuances of stroke severity, navigating the landscape of treatment decisions, or envisioning the long-term recovery outlook, the NIH Stroke Scale numbers served as a guiding compass throughout our discourse. We encourage you to delve deeper into the wealth of knowledge surrounding stroke management and explore the countless ways in which these numbers contribute to the advancement of patient care. As the healthcare landscape continues to evolve, the significance of the NIH Scale remains undeniable, influencing emergency responses, treatment modalities, and rehabilitation strategies. Thank you for accompanying us on this insightful journey, and we look forward to continuing our shared exploration of the multifaceted world of healthcare.
Questions and Answer for NIH Stroke Scale numbers
Q: What is the NIH Stroke Scale?
- The NIH Stroke Scale is a standardized tool used by healthcare professionals to assess and quantify the severity of a stroke.
- It consists of 15 neurological assessments, evaluating various aspects of a patient's cognitive and motor functions.
- The results provide a numeric score that guides emergency responses, treatment decisions, and long-term recovery strategies.
Q: How is the NIH Stroke Scale used in emergency situations?
- During emergencies, the NIH Scale helps healthcare teams rapidly assess the severity of a stroke using its comprehensive set of evaluations.
- The numerical score obtained assists in making swift decisions, ensuring timely interventions tailored to the specific neurological impairment indicated by the scale.
- This immediate response is crucial for mitigating the impact of a stroke and improving patient outcomes.
Q: What role do NIH Stroke Scale numbers play in treatment decisions?
- NIH Stroke Scale numbers play a crucial role in guiding treatment decisions by providing an objective measure of neurological impairment.
- Healthcare professionals use these numbers to tailor interventions, selecting the most appropriate therapies based on the severity indicated by the scale.
- This personalized approach ensures that treatments align with the unique needs of each patient for more effective outcomes.
Q: How do NIH Stroke Scale numbers contribute to long-term recovery?
- When it comes to long-term recovery, NIH Scale numbers inform the development of targeted rehabilitation strategies.
- These numbers help healthcare professionals address specific neurological deficits, optimizing the rehabilitation process for improved, personalized outcomes.
- By anticipating challenges and tailoring interventions, the NIH Stroke Scale plays a key role in shaping a favorable long-term recovery outlook for stroke survivors.
Label :NIH Stroke Scale, Healthcare Assessment, Emergency Response, Patient Care
Keyword : NIH Stroke Scale numbers

Explore the pivotal role of NIH Stroke Scale numbers in deciphering stroke severity. Gain insights for informed healthcare decisions and better patient outcomes.
In the intricate tapestry of healthcare, NIH Stroke Scale numbers emerge as crucial indicators, akin to the silent language spoken by the human body in moments of medical uncertainty. These numeric representations not only unlock a profound understanding of the severity of a stroke but also serve as a compass guiding healthcare professionals through the intricate maze of treatment decisions. As we delve into the corridors of healthcare discourse, this article embarks on a journey to decipher the significance of NIH Stroke Scale numbers, unveiling their nuanced role in the realm of patient care and medical decision-making. Our exploration will navigate through the intricate landscape of stroke assessment, shedding light on the meticulous evaluations encapsulated by these numbers and their pivotal role in shaping the trajectory of recovery for those affected. Join us on this insightful expedition, as we unravel the layers of medical intricacy, connecting the dots between NIH Stroke Scale numbers and the broader healthcare narrative.
Top 10 Points about NIH Stroke Scale numbers :
- Understanding the Significance of NIH Stroke Scale Numbers
- Interpreting Stroke Severity: A Deep Dive into NIH Scale
- How NIH Scale Numbers Guide Emergency Medical Response
- The Crucial Role of NIH Stroke Scale in Treatment Decision-Making
- Measuring Neurological Impairment: NIH Scale in Focus
- Navigating the Landscape of Stroke Assessment with NIH Numbers
- Unraveling the Complexity: NIH Stroke Scale in Patient Care
- NIH Scale Numbers: A Roadmap for Rehabilitation Strategies
- Connecting the Dots: NIH Scale and Long-Term Recovery Outlook
- Enhancing Healthcare Precision: Harnessing NIH Stroke Scale Insights
Several facts about NIH Stroke Scale numbers
Introduction: The NIH Stroke Scale numbers serve as a crucial framework in the realm of healthcare, providing a standardized method to assess and quantify the severity of a stroke. This comprehensive scale enables healthcare professionals to make informed decisions regarding patient care and treatment strategies. As we navigate through the intricacies of stroke assessment, let's delve into the profound implications of NIH Stroke Scale numbers on healthcare outcomes.

Deciphering the NIH Stroke Scale:
The NIH Stroke Scale comprises a set of 15 neurological assessments, meticulously designed to evaluate a patient's cognitive and motor functions. These assessments, ranging from assessing consciousness to motor responses, provide a standardized language for healthcare practitioners to communicate effectively about a patient's condition and determine the severity of a stroke.

Emergency Response and NIH Numbers:
When seconds count, understanding NIH Stroke Scale numbers becomes paramount in shaping the emergency medical response. Rapid assessment using this scale assists emergency medical teams in making swift decisions, ensuring timely interventions to mitigate the impact of a stroke and enhance the chances of a positive outcome.

Treatment Decision-Making:
The role of NIH Stroke Scale numbers extends beyond assessment; it serves as a guiding compass in treatment decision-making. Healthcare professionals leverage these numbers to tailor interventions, choosing the most appropriate therapies based on the severity of neurological impairment indicated by the scale.

Stroke Assessment Landscape:
NIH Stroke Scale numbers play a pivotal role in navigating the complex landscape of stroke assessment. Whether in a hospital setting or during post-stroke rehabilitation, these numbers facilitate communication among healthcare providers, ensuring a cohesive approach to patient care and rehabilitation strategies.
Patient Care and the NIH Scale:
At the heart of patient care lies the meticulous evaluation encapsulated by NIH Stroke Scale numbers. These numbers enable healthcare professionals to tailor their approach, ensuring that each patient receives personalized care that addresses their specific neurological needs, ultimately fostering a more effective and compassionate healthcare environment.

Rehabilitation Strategies:
As patients embark on the journey of recovery, NIH Stroke Scale numbers continue to guide healthcare practitioners in shaping rehabilitation strategies. These numbers inform the development of targeted interventions, optimizing the rehabilitation process and improving the long-term outcomes for individuals affected by strokes.

Long-Term Recovery Outlook:
Connecting the dots between NIH Stroke Scale numbers and the long-term recovery outlook provides a holistic understanding of the patient's journey. Healthcare professionals leverage these numbers to predict and address potential challenges, ensuring a comprehensive and supportive approach to post-stroke care.

Conclusion: In conclusion, the NIH Stroke Scale numbers stand as a cornerstone in the healthcare landscape, offering a standardized and objective tool for assessing and managing stroke severity. The integration of these numbers into medical practices not only enhances emergency response and treatment decisions but also paves the way for a more personalized and effective approach to patient care and rehabilitation.
Sources: (Add sources and references here, using proper citation format.)
NIH Stroke Scale numbers in Professional's eye
In the intricate realm of healthcare, the
NIH Stroke Scale numbers serve as a linchpin in the standardized assessment of stroke severity, providing clinicians with a comprehensive toolset to navigate the complexities of neurological impairment. As we delve into the profound implications of this scale, it becomes evident that the structured evaluation it offers plays a pivotal role in shaping emergency responses, treatment decisions, and long-term patient outcomes.
Deciphering the NIH Stroke Scale, the foundation of stroke assessment, involves a meticulous examination of 15 neurological parameters, each contributing to a nuanced understanding of a patient's cognitive and motor functions. This standardized language, akin to a diagnostic lexicon, facilitates effective communication among healthcare professionals, fostering a shared understanding of a patient's condition.

Moving beyond assessment, the connection between
NIH Stroke Scale numbers and
emergency response is palpable. In the high-stakes arena of stroke management, swift decision-making is paramount. The NIH Scale serves as a rapid diagnostic aid, enabling emergency medical teams to swiftly intervene and administer appropriate treatments based on the severity of neurological impairment indicated by the scale. This immediate response is crucial in mitigating the potentially devastating effects of a stroke and significantly impacting patient outcomes.

As healthcare professionals navigate the labyrinth of treatment decisions, the influence of
NIH Stroke Scale numbers becomes increasingly evident. The scale becomes a guiding compass, aiding clinicians in tailoring interventions based on the severity of the neurological deficit. This personalized approach ensures that treatments are not only effective but are also aligned with the unique needs of each patient. The integration of NIH Scale data into treatment decisions fosters a more nuanced and patient-centric approach to stroke care, emphasizing the importance of individualized therapeutic strategies.

Navigating the broader landscape of
stroke assessment, the NIH Scale numbers provide a standardized framework for healthcare providers. Whether in a bustling emergency room or a rehabilitation setting, these numbers enable seamless communication and understanding among multidisciplinary teams. The scale transcends the confines of individual specialties, serving as a common language that facilitates collaboration and ensures a cohesive approach to patient care. In essence, the NIH Stroke Scale becomes a unifying force, connecting professionals across various healthcare domains in their shared mission to optimize patient outcomes.
At the heart of patient care lies the meticulous evaluation encapsulated by
NIH Stroke Scale numbers. This holistic approach extends beyond immediate interventions, encompassing the entirety of a patient's journey towards recovery. The scale acts as a guiding light, helping healthcare providers navigate the complexities of post-stroke care. By leveraging NIH Scale data, professionals can tailor rehabilitation strategies to address specific neurological deficits, ensuring a more effective and targeted approach to recovery. The integration of these numbers into the fabric of patient care represents a commitment to not only treating the immediate consequences of a stroke but also fostering long-term well-being.

As patients embark on the path of rehabilitation, the role of
NIH Stroke Scale numbers in shaping
rehabilitation strategies becomes increasingly pronounced. Each numeric value serves as a roadmap, guiding healthcare professionals in the development of tailored interventions that address the unique challenges posed by a stroke. By harnessing the insights provided by the NIH Scale, rehabilitation efforts become more targeted, efficient, and patient-centered. This strategic approach not only optimizes the rehabilitation process but also contributes to improved long-term outcomes for individuals on their journey towards recovery.

Connecting the dots between
NIH Stroke Scale numbers and the
long-term recovery outlook unveils a comprehensive understanding of the patient's trajectory post-stroke. Healthcare professionals use these numbers to anticipate potential challenges, enabling proactive interventions that contribute to a more favorable recovery prognosis. This foresight, rooted in the objective data provided by the NIH Scale, becomes instrumental in shaping a holistic and supportive approach to long-term care.

In conclusion, the
NIH Stroke Scale numbers emerge as a cornerstone in the healthcare landscape, offering a standardized and objective framework for assessing and managing stroke severity. From the initial emergency response to the intricate web of treatment decisions and the long-term journey of recovery, these numbers serve as a guiding thread. The integration of NIH Scale data into medical practices not only enhances emergency response and treatment decisions but also paves the way for a more personalized and effective approach to patient care and rehabilitation. As healthcare continues to advance, the NIH Stroke Scale remains an invaluable tool, contributing to the evolution of stroke management and the overall improvement of patient outcomes.
Sources: (Add sources and references here, using proper citation format.)
Point of Views : NIH Stroke Scale numbers
1. In the grand theater of healthcare, where the drama unfolds with heartbeats and stethoscopes, the
NIH Stroke Scale numbers take center stage. Picture it as a blockbuster movie, where the protagonist is a set of carefully curated neurological assessments, each with its own quirks and intricacies, coming together to create a cinematic masterpiece of stroke severity evaluation.
2. Forget Sherlock Holmes; when it comes to unraveling the mystery of neurological impairment, our unsung hero is the NIH Scale. It's like having a detective with 15 different magnifying glasses, each probing a different aspect of cognitive and motor functions. Talk about thorough investigative work – Hercule Poirot would be proud!
3. Now, let's talk emergency response, where speed is of the essence. The NIH Stroke Scale is like the Flash of the medical world, zipping through assessments faster than you can say "Is it a bird? Is it a plane?" Swift and precise, it's the superhero we need when time is ticking away.
4. Treatment decisions become a strategic game of chess, and the NIH Scale is the grandmaster making moves based on
NIH Stroke Scale numbers. Each number is a pawn, knight, or queen on the chessboard, influencing the course of the game – or in this case, the patient's journey. Checkmate to neurological impairment!
5. Entering the realm of
stroke assessment, it's like a medical symphony where each instrument plays a crucial role. The NIH Stroke Scale becomes the conductor, ensuring that every healthcare professional is reading from the same sheet of music. Harmony in healthcare? Who would've thought?
6. Patient care takes on an almost poetic quality with the NIH Scale. It's not just about numbers; it's about understanding the language of the body and responding with the precision of a Shakespearean sonnet. To be or not to be in neurological distress – that is the question answered by the NIH Scale.
7. Rehabilitation strategies, when guided by
NIH Stroke Scale numbers, become a carefully choreographed dance. It's not just about making movements; it's about hitting the right steps at the right time. Think of it as healthcare's version of Dancing with the Stars – a graceful journey towards recovery.
8. Long-term recovery outlook becomes the grand finale, and the NIH Scale is the fireworks display. It lights up the sky with predictions, allowing healthcare professionals to anticipate challenges and celebrate victories. Who knew a set of numbers could make healthcare feel like a dazzling fireworks show?
9. In the end, the NIH Stroke Scale numbers aren't just digits on a chart; they are the protagonists, superheroes, conductors, poets, dancers, and pyrotechnicians of the healthcare world. They turn the serious business of stroke management into a blockbuster performance, leaving a lasting impact on patient outcomes.
10. So, next time you hear about the NIH Stroke Scale, don't just think of it as a set of numbers; think of it as the lead actor in the healthcare drama, delivering a performance that can rival even the most captivating blockbuster. After all, laughter might be the best medicine, but a bit of drama with
NIH Stroke Scale numbers comes in at a close second!
Conclusion :As we draw the curtains on our exploration of the NIH Stroke Scale numbers, we hope this journey has illuminated the intricacies of stroke assessment and underscored the critical role these numbers play in healthcare. From the initial evaluation of neurological impairment to the formulation of treatment strategies, the NIH Scale emerges as a foundational tool, providing a standardized and objective framework for healthcare professionals. Our venture into the world of emergency response showcased how these numbers become a rallying point for swift and effective interventions, ensuring timely and targeted care for stroke patients.
Whether you found yourself deciphering the nuances of stroke severity, navigating the landscape of treatment decisions, or envisioning the long-term recovery outlook, the NIH Stroke Scale numbers served as a guiding compass throughout our discourse. We encourage you to delve deeper into the wealth of knowledge surrounding stroke management and explore the countless ways in which these numbers contribute to the advancement of patient care. As the healthcare landscape continues to evolve, the significance of the NIH Scale remains undeniable, influencing emergency responses, treatment modalities, and rehabilitation strategies. Thank you for accompanying us on this insightful journey, and we look forward to continuing our shared exploration of the multifaceted world of healthcare.
Questions and Answer for NIH Stroke Scale numbers
Q: What is the NIH Stroke Scale?
- The NIH Stroke Scale is a standardized tool used by healthcare professionals to assess and quantify the severity of a stroke.
- It consists of 15 neurological assessments, evaluating various aspects of a patient's cognitive and motor functions.
- The results provide a numeric score that guides emergency responses, treatment decisions, and long-term recovery strategies.
Q: How is the NIH Stroke Scale used in emergency situations?
- During emergencies, the NIH Scale helps healthcare teams rapidly assess the severity of a stroke using its comprehensive set of evaluations.
- The numerical score obtained assists in making swift decisions, ensuring timely interventions tailored to the specific neurological impairment indicated by the scale.
- This immediate response is crucial for mitigating the impact of a stroke and improving patient outcomes.
Q: What role do NIH Stroke Scale numbers play in treatment decisions?
- NIH Stroke Scale numbers play a crucial role in guiding treatment decisions by providing an objective measure of neurological impairment.
- Healthcare professionals use these numbers to tailor interventions, selecting the most appropriate therapies based on the severity indicated by the scale.
- This personalized approach ensures that treatments align with the unique needs of each patient for more effective outcomes.
Q: How do NIH Stroke Scale numbers contribute to long-term recovery?
- When it comes to long-term recovery, NIH Scale numbers inform the development of targeted rehabilitation strategies.
- These numbers help healthcare professionals address specific neurological deficits, optimizing the rehabilitation process for improved, personalized outcomes.
- By anticipating challenges and tailoring interventions, the NIH Stroke Scale plays a key role in shaping a favorable long-term recovery outlook for stroke survivors.
Label :NIH Stroke Scale, Healthcare Assessment, Emergency Response, Patient Care
Keyword : NIH Stroke Scale numbers
0 komentar