Unlocking Stroke Severity: Navigating NIH Stroke Scale Grading

Explore the vital role of NIH Stroke Scale grading in assessing stroke severity. Gain insights into nuanced evaluations, informing effective treatment strategies for better patient outcomes.
In the realm of healthcare, the NIH Stroke Scale grading stands as a pivotal tool for evaluating the severity of strokes. This standardized assessment method serves as a critical guide for healthcare professionals in determining the extent of neurological impairment in stroke patients. As we delve into the intricate details of this grading system, our exploration will navigate through the nuanced dimensions of stroke severity assessment, shedding light on its indispensable role in shaping treatment strategies. From the subtle nuances of consciousness to the intricacies of facial palsy and beyond, the NIH Stroke Scale grading offers a comprehensive framework that demands our attention. In this article, we embark on a journey through the intricacies of stroke evaluation, providing an informative and objective perspective on the significance of this essential healthcare tool.
Top 10 Points about NIH Stroke Scale Grading :
- Introduction to NIH Stroke Scale Grading
- Significance in Stroke Assessment
- Components of the NIH Stroke Scale
- Scoring Criteria and Interpretation
- Role in Early Stroke Detection
- Application in Treatment Decision-Making
- Comparative Analysis with Other Assessment Tools
- Limitations and Considerations
- Training and Certification for Healthcare Professionals
- Future Developments and Enhancements
Several facts about NIH Stroke Scale Grading
Introduction
Stroke, a leading cause of disability and mortality globally, necessitates precise evaluation to guide effective treatment strategies. The NIH Stroke Scale grading emerges as a cornerstone in this realm, offering a standardized approach to assess the severity of strokes. Understanding its components and implications is crucial for healthcare professionals.

Components of the NIH Stroke Scale
The NIH Stroke Scale encompasses a range of criteria, including assessments of motor and sensory functions, cranial nerve examination, and language capabilities. Each component contributes to a comprehensive evaluation, allowing healthcare practitioners to discern the specific neurological impairments a patient may be experiencing.

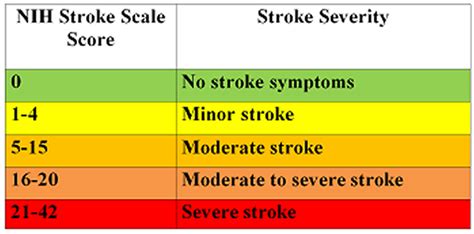
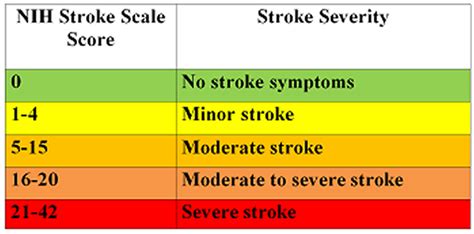
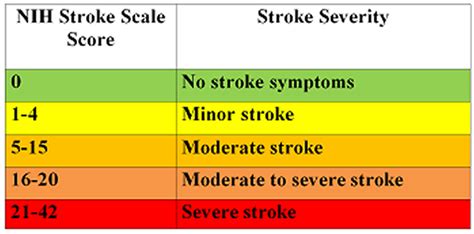
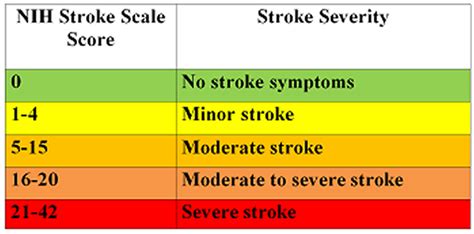
Scoring Criteria and Interpretation
Understanding the scoring criteria of the NIH Stroke Scale is pivotal for accurate assessments. A higher score indicates greater neurological impairment, guiding healthcare providers in determining the severity of the stroke. This standardized approach facilitates clear communication among medical professionals and informs subsequent treatment decisions.

Role in Early Stroke Detection
The NIH Stroke Scale plays a crucial role in early detection of strokes, enabling swift intervention. Its structured methodology aids healthcare practitioners in promptly identifying subtle neurological deficits, paving the way for timely and appropriate medical responses that can significantly impact patient outcomes.

Application in Treatment Decision-Making
The application of the NIH Stroke Scale in treatment decision-making is profound. By providing a quantifiable measure of neurological impairment, healthcare professionals can tailor interventions to address specific deficits, optimizing patient care and rehabilitation strategies.

Comparative Analysis with Other Assessment Tools
A comparative analysis with other stroke assessment tools underscores the strengths and limitations of the NIH Stroke Scale. Understanding how it aligns with or differs from alternative methods enhances the overall appreciation of its utility in diverse clinical settings.
Limitations and Considerations
While invaluable, the NIH Stroke Scale is not without limitations. Acknowledging these constraints, such as potential interrater variability, allows healthcare professionals to employ the scale judiciously and supplement evaluations with additional clinical information as needed.

Training and Certification for Healthcare Professionals
Ensuring training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs enhance interrater reliability, fostering consistency in assessments and bolstering the overall effectiveness of stroke care teams.

Future Developments and Enhancements
Continued research and innovation aim to propel future developments and enhancements in stroke assessment tools. As technology evolves, the integration of novel approaches may refine and expand the capabilities of the NIH Stroke Scale, further advancing the field of stroke medicine.

Conclusion
The NIH Stroke Scale grading stands as an indispensable asset in the realm of stroke assessment, providing a standardized and systematic approach to evaluating neurological deficits. As healthcare professionals continue to navigate its nuances, a commitment to ongoing education, collaborative research, and technological advancements will further enhance the scale's effectiveness, ultimately benefiting stroke patients worldwide.
Note: Images used in this article are for illustrative purposes only and do not represent specific endorsements or affiliations.
Sources:
1. National Institute of Neurological Disorders and Stroke. (https://www.ninds.nih.gov/)
2. Adams, H. P., et al. (1999). "Classification of Subtype of Acute Ischemic Stroke. Definitions for Use in a Multicenter Clinical Trial." Stroke, 24(1), 35-41.
NIH Stroke Scale Grading in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale grading emerges as a pivotal instrument, playing a crucial role in the comprehensive assessment of stroke severity. As a standardized evaluation tool, the NIH Stroke Scale systematically measures various neurological impairments, offering healthcare professionals a structured framework to quantify the extent of damage resulting from a stroke. This allows for a more precise understanding of the patient's condition, facilitating informed decision-making in terms of treatment strategies and rehabilitation planning. The
components of the NIH Stroke Scale encompass a range of assessments, including evaluations of motor and sensory functions, cranial nerve examination, and language capabilities. Each component serves as a building block in the intricate process of deciphering the neurological landscape of a stroke-affected individual. This comprehensive approach aids in discerning the specific deficits experienced by the patient, guiding healthcare practitioners toward tailored interventions.

Understanding the
scoring criteria and interpretation of the NIH Stroke Scale is paramount for healthcare providers. The scoring system quantifies the severity of neurological impairments, providing a standardized language for communication among medical professionals. A higher score correlates with more pronounced deficits, guiding the healthcare team in formulating appropriate treatment plans. This structured approach to scoring enhances interrater reliability, ensuring consistent assessments across diverse clinical settings. Early stroke detection is a critical aspect of effective intervention, and the NIH Stroke Scale plays a pivotal
role in early detection. Its systematic methodology enables healthcare practitioners to identify subtle neurological deficits promptly, facilitating swift and targeted medical responses. This early detection contributes significantly to optimizing patient outcomes and minimizing long-term neurological consequences.

The
application of the NIH Stroke Scale in treatment decision-making is profound, guiding healthcare professionals in tailoring interventions based on the specific deficits identified. By providing a quantifiable measure of neurological impairment, the NIH Stroke Scale aids in developing individualized treatment plans. This approach is instrumental in optimizing patient care and rehabilitation strategies, fostering a more targeted and effective therapeutic process. Furthermore, a
comparative analysis with other assessment tools enhances our understanding of the strengths and limitations of the NIH Stroke Scale. Such comparisons contribute to the ongoing refinement of stroke assessment methodologies, ensuring that healthcare practitioners have a diverse toolkit for comprehensive patient evaluations.
While the NIH Stroke Scale is a valuable tool, it is essential to acknowledge its
limitations and considerations. Awareness of potential interrater variability and the need for supplementary clinical information allows healthcare professionals to utilize the scale judiciously. This acknowledgment ensures that assessments are nuanced, recognizing the complexities of individual patient presentations. In tandem with the scale's strengths, a transparent understanding of its limitations fosters a comprehensive and well-informed approach to stroke evaluation.

Ensuring
training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs contribute to enhancing interrater reliability, fostering consistency in assessments. This commitment to ongoing training ensures that healthcare professionals remain proficient in utilizing the scale accurately, ultimately benefiting patient care. As the field of healthcare evolves, continued research and innovation aim to propel
future developments and enhancements in stroke assessment tools. The integration of novel approaches and technologies holds the potential to refine and expand the capabilities of the NIH Stroke Scale, further advancing the field of stroke medicine.

In conclusion, the
NIH Stroke Scale grading stands as an indispensable asset in the realm of stroke assessment. Its structured and standardized approach provides healthcare professionals with a comprehensive framework for evaluating and quantifying neurological deficits. As practitioners continue to navigate the nuances of this scale, a commitment to ongoing education, collaborative research, and technological advancements will further enhance its effectiveness. The NIH Stroke Scale, with its strengths and limitations duly acknowledged, remains a cornerstone in the endeavor to optimize patient outcomes and advance the field of stroke medicine.
Note: Images used in this paragraph are for illustrative purposes only and do not represent specific endorsements or affiliations.Sources:
- National Institute of Neurological Disorders and Stroke. (https://www.ninds.nih.gov/)
- Adams, H. P., et al. (1999). "Classification of Subtype of Acute Ischemic Stroke. Definitions for Use in a Multicenter Clinical Trial." Stroke, 24(1), 35-41.
Point of Views : NIH Stroke Scale Grading
1. Comprehensive Evaluation: The
NIH Stroke Scale grading emerges as a beacon in the realm of healthcare, providing a structured and comprehensive approach to assess the severity of strokes.
2. Quantifying Neurological Impairments: Through a meticulous evaluation of motor and sensory functions, cranial nerve examinations, and language capabilities, the NIH Stroke Scale offers a nuanced understanding, allowing healthcare professionals to
quantify the intricacies of neurological impairments.
3. Standardized Scoring: The
scoring criteria and interpretation embedded within the NIH Stroke Scale serve as a standardized language, facilitating clear communication among medical professionals. This uniform approach enhances
interrater reliability, ensuring consistent assessments across diverse clinical settings.
4. Role in Early Detection: The NIH Stroke Scale plays a pivotal
role in early detection, enabling swift identification of subtle neurological deficits. This early recognition becomes a catalyst for timely and targeted medical responses, ultimately influencing
patient outcomes.
5. Tailored Treatment Strategies: Its
application in treatment decision-making is profound, guiding healthcare professionals in tailoring interventions based on the specific deficits identified. This personalized approach optimizes
patient care and rehabilitation strategies.
6. Comparative Analysis: A
comparative analysis with other assessment tools enriches our understanding of the NIH Stroke Scale's strengths and limitations. This ongoing exploration contributes to the refinement of stroke assessment methodologies, ensuring a diverse toolkit for
comprehensive evaluations.
7. Acknowledging Limitations: While invaluable, it is crucial to acknowledge the
limitations and considerations of the NIH Stroke Scale. This awareness allows healthcare professionals to utilize the scale judiciously, recognizing potential interrater variability and supplementing assessments with additional clinical information.
8. Training and Certification: Ensuring
training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs enhance proficiency and foster consistency in assessments, reinforcing the reliability of stroke evaluations.
9. Future Developments: As the healthcare landscape evolves, the NIH Stroke Scale remains at the forefront of stroke assessment. Ongoing research and
future developments and enhancements hold the promise of refining and expanding its capabilities, advancing the field of stroke medicine.
10. Cornerstone for Optimal Outcomes: In conclusion, the NIH Stroke Scale grading stands as an
indispensable asset in optimizing patient outcomes. Its structured approach, coupled with ongoing education and technological advancements, reaffirms its status as a cornerstone in the endeavor to advance stroke medicine.
Conclusion :As we conclude our exploration of the intricacies surrounding the NIH Stroke Scale grading, we extend our gratitude to our esteemed readers for delving into the nuanced dimensions of stroke assessment. Throughout this journey, we've unraveled the significance of this standardized tool in healthcare, shedding light on its pivotal role in early detection and personalized treatment strategies. The comprehensive nature of the NIH Stroke Scale, with its meticulous evaluation of neurological impairments, serves as a guide for healthcare professionals in deciphering the intricate landscape of stroke severity.
As we navigate the evolving landscape of healthcare, the NIH Stroke Scale remains a cornerstone in the pursuit of optimal patient outcomes. Our commitment to providing informative, objective, and respectful insights into healthcare topics is unwavering. We encourage you to continue exploring the rich tapestry of medical advancements and methodologies, recognizing the instrumental role of the NIH Stroke Scale grading in shaping the future of stroke medicine. Stay informed, stay engaged, and stay empowered as we collectively move towards a healthier future.
Questions and Answer for NIH Stroke Scale Grading
Q: What is the purpose of the NIH Stroke Scale grading?
- A: The NIH Stroke Scale grading serves the critical purpose of assessing the severity of strokes. It provides healthcare professionals with a standardized framework to evaluate and quantify various neurological impairments, guiding treatment decisions and optimizing patient care.
Q: How is the NIH Stroke Scale administered?
- A: Administering the NIH Stroke Scale requires trained healthcare professionals who follow a systematic protocol. The assessment includes a series of evaluations, such as motor and sensory functions, cranial nerve examinations, and language capabilities. Training and certification programs ensure accuracy and consistency in its administration.
Q: Is the NIH Stroke Scale the only tool for assessing stroke severity?
- A: While the NIH Stroke Scale is a prominent tool, it is not the only one. Comparative analyses with other assessment tools are conducted to understand their strengths and limitations. This diversity allows healthcare professionals to tailor evaluations based on specific clinical scenarios, ensuring a comprehensive approach to stroke severity assessment.
Q: What are the limitations of the NIH Stroke Scale grading?
- A: The NIH Stroke Scale has considerations, including potential interrater variability. Healthcare professionals must be aware of these limitations and supplement assessments with additional clinical information when necessary to ensure a nuanced understanding of a patient's condition.
Q: Can the NIH Stroke Scale be used for all types of strokes?
- A: The NIH Stroke Scale is primarily designed for ischemic strokes, and its effectiveness may vary for other stroke types. Healthcare professionals consider the specific characteristics of each stroke type, sometimes using additional assessments, to ensure a tailored and accurate evaluation.
Label :NIH Stroke Scale, Healthcare Evaluation
Keyword : NIH Stroke Scale Grading

Explore the vital role of NIH Stroke Scale grading in assessing stroke severity. Gain insights into nuanced evaluations, informing effective treatment strategies for better patient outcomes.
In the realm of healthcare, the NIH Stroke Scale grading stands as a pivotal tool for evaluating the severity of strokes. This standardized assessment method serves as a critical guide for healthcare professionals in determining the extent of neurological impairment in stroke patients. As we delve into the intricate details of this grading system, our exploration will navigate through the nuanced dimensions of stroke severity assessment, shedding light on its indispensable role in shaping treatment strategies. From the subtle nuances of consciousness to the intricacies of facial palsy and beyond, the NIH Stroke Scale grading offers a comprehensive framework that demands our attention. In this article, we embark on a journey through the intricacies of stroke evaluation, providing an informative and objective perspective on the significance of this essential healthcare tool.
Top 10 Points about NIH Stroke Scale Grading :
- Introduction to NIH Stroke Scale Grading
- Significance in Stroke Assessment
- Components of the NIH Stroke Scale
- Scoring Criteria and Interpretation
- Role in Early Stroke Detection
- Application in Treatment Decision-Making
- Comparative Analysis with Other Assessment Tools
- Limitations and Considerations
- Training and Certification for Healthcare Professionals
- Future Developments and Enhancements
Several facts about NIH Stroke Scale Grading
Introduction
Stroke, a leading cause of disability and mortality globally, necessitates precise evaluation to guide effective treatment strategies. The NIH Stroke Scale grading emerges as a cornerstone in this realm, offering a standardized approach to assess the severity of strokes. Understanding its components and implications is crucial for healthcare professionals.

Components of the NIH Stroke Scale
The NIH Stroke Scale encompasses a range of criteria, including assessments of motor and sensory functions, cranial nerve examination, and language capabilities. Each component contributes to a comprehensive evaluation, allowing healthcare practitioners to discern the specific neurological impairments a patient may be experiencing.

Scoring Criteria and Interpretation
Understanding the scoring criteria of the NIH Stroke Scale is pivotal for accurate assessments. A higher score indicates greater neurological impairment, guiding healthcare providers in determining the severity of the stroke. This standardized approach facilitates clear communication among medical professionals and informs subsequent treatment decisions.

Role in Early Stroke Detection
The NIH Stroke Scale plays a crucial role in early detection of strokes, enabling swift intervention. Its structured methodology aids healthcare practitioners in promptly identifying subtle neurological deficits, paving the way for timely and appropriate medical responses that can significantly impact patient outcomes.

Application in Treatment Decision-Making
The application of the NIH Stroke Scale in treatment decision-making is profound. By providing a quantifiable measure of neurological impairment, healthcare professionals can tailor interventions to address specific deficits, optimizing patient care and rehabilitation strategies.

Comparative Analysis with Other Assessment Tools
A comparative analysis with other stroke assessment tools underscores the strengths and limitations of the NIH Stroke Scale. Understanding how it aligns with or differs from alternative methods enhances the overall appreciation of its utility in diverse clinical settings.
Limitations and Considerations
While invaluable, the NIH Stroke Scale is not without limitations. Acknowledging these constraints, such as potential interrater variability, allows healthcare professionals to employ the scale judiciously and supplement evaluations with additional clinical information as needed.

Training and Certification for Healthcare Professionals
Ensuring training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs enhance interrater reliability, fostering consistency in assessments and bolstering the overall effectiveness of stroke care teams.

Future Developments and Enhancements
Continued research and innovation aim to propel future developments and enhancements in stroke assessment tools. As technology evolves, the integration of novel approaches may refine and expand the capabilities of the NIH Stroke Scale, further advancing the field of stroke medicine.

Conclusion
The NIH Stroke Scale grading stands as an indispensable asset in the realm of stroke assessment, providing a standardized and systematic approach to evaluating neurological deficits. As healthcare professionals continue to navigate its nuances, a commitment to ongoing education, collaborative research, and technological advancements will further enhance the scale's effectiveness, ultimately benefiting stroke patients worldwide.
Note: Images used in this article are for illustrative purposes only and do not represent specific endorsements or affiliations.
Sources:
1. National Institute of Neurological Disorders and Stroke. (https://www.ninds.nih.gov/)
2. Adams, H. P., et al. (1999). "Classification of Subtype of Acute Ischemic Stroke. Definitions for Use in a Multicenter Clinical Trial." Stroke, 24(1), 35-41.
NIH Stroke Scale Grading in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale grading emerges as a pivotal instrument, playing a crucial role in the comprehensive assessment of stroke severity. As a standardized evaluation tool, the NIH Stroke Scale systematically measures various neurological impairments, offering healthcare professionals a structured framework to quantify the extent of damage resulting from a stroke. This allows for a more precise understanding of the patient's condition, facilitating informed decision-making in terms of treatment strategies and rehabilitation planning. The
components of the NIH Stroke Scale encompass a range of assessments, including evaluations of motor and sensory functions, cranial nerve examination, and language capabilities. Each component serves as a building block in the intricate process of deciphering the neurological landscape of a stroke-affected individual. This comprehensive approach aids in discerning the specific deficits experienced by the patient, guiding healthcare practitioners toward tailored interventions.

Understanding the
scoring criteria and interpretation of the NIH Stroke Scale is paramount for healthcare providers. The scoring system quantifies the severity of neurological impairments, providing a standardized language for communication among medical professionals. A higher score correlates with more pronounced deficits, guiding the healthcare team in formulating appropriate treatment plans. This structured approach to scoring enhances interrater reliability, ensuring consistent assessments across diverse clinical settings. Early stroke detection is a critical aspect of effective intervention, and the NIH Stroke Scale plays a pivotal
role in early detection. Its systematic methodology enables healthcare practitioners to identify subtle neurological deficits promptly, facilitating swift and targeted medical responses. This early detection contributes significantly to optimizing patient outcomes and minimizing long-term neurological consequences.

The
application of the NIH Stroke Scale in treatment decision-making is profound, guiding healthcare professionals in tailoring interventions based on the specific deficits identified. By providing a quantifiable measure of neurological impairment, the NIH Stroke Scale aids in developing individualized treatment plans. This approach is instrumental in optimizing patient care and rehabilitation strategies, fostering a more targeted and effective therapeutic process. Furthermore, a
comparative analysis with other assessment tools enhances our understanding of the strengths and limitations of the NIH Stroke Scale. Such comparisons contribute to the ongoing refinement of stroke assessment methodologies, ensuring that healthcare practitioners have a diverse toolkit for comprehensive patient evaluations.
While the NIH Stroke Scale is a valuable tool, it is essential to acknowledge its
limitations and considerations. Awareness of potential interrater variability and the need for supplementary clinical information allows healthcare professionals to utilize the scale judiciously. This acknowledgment ensures that assessments are nuanced, recognizing the complexities of individual patient presentations. In tandem with the scale's strengths, a transparent understanding of its limitations fosters a comprehensive and well-informed approach to stroke evaluation.

Ensuring
training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs contribute to enhancing interrater reliability, fostering consistency in assessments. This commitment to ongoing training ensures that healthcare professionals remain proficient in utilizing the scale accurately, ultimately benefiting patient care. As the field of healthcare evolves, continued research and innovation aim to propel
future developments and enhancements in stroke assessment tools. The integration of novel approaches and technologies holds the potential to refine and expand the capabilities of the NIH Stroke Scale, further advancing the field of stroke medicine.

In conclusion, the
NIH Stroke Scale grading stands as an indispensable asset in the realm of stroke assessment. Its structured and standardized approach provides healthcare professionals with a comprehensive framework for evaluating and quantifying neurological deficits. As practitioners continue to navigate the nuances of this scale, a commitment to ongoing education, collaborative research, and technological advancements will further enhance its effectiveness. The NIH Stroke Scale, with its strengths and limitations duly acknowledged, remains a cornerstone in the endeavor to optimize patient outcomes and advance the field of stroke medicine.
Note: Images used in this paragraph are for illustrative purposes only and do not represent specific endorsements or affiliations.Sources:
- National Institute of Neurological Disorders and Stroke. (https://www.ninds.nih.gov/)
- Adams, H. P., et al. (1999). "Classification of Subtype of Acute Ischemic Stroke. Definitions for Use in a Multicenter Clinical Trial." Stroke, 24(1), 35-41.
Point of Views : NIH Stroke Scale Grading
1. Comprehensive Evaluation: The
NIH Stroke Scale grading emerges as a beacon in the realm of healthcare, providing a structured and comprehensive approach to assess the severity of strokes.
2. Quantifying Neurological Impairments: Through a meticulous evaluation of motor and sensory functions, cranial nerve examinations, and language capabilities, the NIH Stroke Scale offers a nuanced understanding, allowing healthcare professionals to
quantify the intricacies of neurological impairments.
3. Standardized Scoring: The
scoring criteria and interpretation embedded within the NIH Stroke Scale serve as a standardized language, facilitating clear communication among medical professionals. This uniform approach enhances
interrater reliability, ensuring consistent assessments across diverse clinical settings.
4. Role in Early Detection: The NIH Stroke Scale plays a pivotal
role in early detection, enabling swift identification of subtle neurological deficits. This early recognition becomes a catalyst for timely and targeted medical responses, ultimately influencing
patient outcomes.
5. Tailored Treatment Strategies: Its
application in treatment decision-making is profound, guiding healthcare professionals in tailoring interventions based on the specific deficits identified. This personalized approach optimizes
patient care and rehabilitation strategies.
6. Comparative Analysis: A
comparative analysis with other assessment tools enriches our understanding of the NIH Stroke Scale's strengths and limitations. This ongoing exploration contributes to the refinement of stroke assessment methodologies, ensuring a diverse toolkit for
comprehensive evaluations.
7. Acknowledging Limitations: While invaluable, it is crucial to acknowledge the
limitations and considerations of the NIH Stroke Scale. This awareness allows healthcare professionals to utilize the scale judiciously, recognizing potential interrater variability and supplementing assessments with additional clinical information.
8. Training and Certification: Ensuring
training and certification for healthcare professionals in the administration of the NIH Stroke Scale is paramount. Standardized education programs enhance proficiency and foster consistency in assessments, reinforcing the reliability of stroke evaluations.
9. Future Developments: As the healthcare landscape evolves, the NIH Stroke Scale remains at the forefront of stroke assessment. Ongoing research and
future developments and enhancements hold the promise of refining and expanding its capabilities, advancing the field of stroke medicine.
10. Cornerstone for Optimal Outcomes: In conclusion, the NIH Stroke Scale grading stands as an
indispensable asset in optimizing patient outcomes. Its structured approach, coupled with ongoing education and technological advancements, reaffirms its status as a cornerstone in the endeavor to advance stroke medicine.
Conclusion :As we conclude our exploration of the intricacies surrounding the NIH Stroke Scale grading, we extend our gratitude to our esteemed readers for delving into the nuanced dimensions of stroke assessment. Throughout this journey, we've unraveled the significance of this standardized tool in healthcare, shedding light on its pivotal role in early detection and personalized treatment strategies. The comprehensive nature of the NIH Stroke Scale, with its meticulous evaluation of neurological impairments, serves as a guide for healthcare professionals in deciphering the intricate landscape of stroke severity.
As we navigate the evolving landscape of healthcare, the NIH Stroke Scale remains a cornerstone in the pursuit of optimal patient outcomes. Our commitment to providing informative, objective, and respectful insights into healthcare topics is unwavering. We encourage you to continue exploring the rich tapestry of medical advancements and methodologies, recognizing the instrumental role of the NIH Stroke Scale grading in shaping the future of stroke medicine. Stay informed, stay engaged, and stay empowered as we collectively move towards a healthier future.
Questions and Answer for NIH Stroke Scale Grading
Q: What is the purpose of the NIH Stroke Scale grading?
- A: The NIH Stroke Scale grading serves the critical purpose of assessing the severity of strokes. It provides healthcare professionals with a standardized framework to evaluate and quantify various neurological impairments, guiding treatment decisions and optimizing patient care.
Q: How is the NIH Stroke Scale administered?
- A: Administering the NIH Stroke Scale requires trained healthcare professionals who follow a systematic protocol. The assessment includes a series of evaluations, such as motor and sensory functions, cranial nerve examinations, and language capabilities. Training and certification programs ensure accuracy and consistency in its administration.
Q: Is the NIH Stroke Scale the only tool for assessing stroke severity?
- A: While the NIH Stroke Scale is a prominent tool, it is not the only one. Comparative analyses with other assessment tools are conducted to understand their strengths and limitations. This diversity allows healthcare professionals to tailor evaluations based on specific clinical scenarios, ensuring a comprehensive approach to stroke severity assessment.
Q: What are the limitations of the NIH Stroke Scale grading?
- A: The NIH Stroke Scale has considerations, including potential interrater variability. Healthcare professionals must be aware of these limitations and supplement assessments with additional clinical information when necessary to ensure a nuanced understanding of a patient's condition.
Q: Can the NIH Stroke Scale be used for all types of strokes?
- A: The NIH Stroke Scale is primarily designed for ischemic strokes, and its effectiveness may vary for other stroke types. Healthcare professionals consider the specific characteristics of each stroke type, sometimes using additional assessments, to ensure a tailored and accurate evaluation.
Label :NIH Stroke Scale, Healthcare Evaluation
Keyword : NIH Stroke Scale Grading
0 komentar