Decoding Facial Palsy: Navigating NIH Stroke Scale for Precise Assessment

Uncover the clinical insights of Facial Palsy with our in-depth exploration of the NIH Stroke Scale. Enhance your understanding for precise stroke-related assessments in comprehensive healthcare.
Facial palsy, a condition characterized by the partial or complete loss of voluntary muscle control on one side of the face, stands as a compelling manifestation of neurological impairment. The significance of its assessment in the context of stroke is underscored by the meticulous NIH Stroke Scale—an instrument meticulously designed for the quantification and documentation of stroke-related impairments. This article delves into the nuanced realm of healthcare, specifically exploring the diagnostic utility and clinical implications of the Facial Palsy NIH Stroke Scale. As we navigate this discourse, a judicious examination of the objective parameters and standardized criteria employed in this evaluation will unravel, elucidating the multifaceted dimensions of facial palsy assessment within the broader landscape of stroke care.
Top 10 Points about Facial palsy NIH Stroke Scale :
- Understanding Facial Palsy: A Brief Overview
- The Role of NIH Stroke Scale in Neurological Assessments
- Facial Palsy as a Clinical Manifestation of Stroke
- Exploring the Anatomy of Facial Nerve in Palsy Cases
- Importance of Early Detection in Facial Palsy Evaluation
- NIH Stroke Scale Criteria for Facial Palsy Grading
- Clinical Implications of Facial Palsy in Stroke Patients
- Relevance of NIH Stroke Scale in Comprehensive Stroke Care
- Interpreting Facial Palsy Scores: A Practical Guide
- Future Directions in Facial Palsy Research and Assessment
Several facts about Facial palsy NIH Stroke Scale
Understanding Facial Palsy

Facial palsy, a condition marked by the weakness or paralysis of facial muscles, serves as a critical indicator of neurological dysfunction. This impairment often results from damage to the facial nerve, leading to challenges in facial movement and expression. Facial palsy is not only a physical manifestation but also a potential consequence of underlying health issues, such as strokes or infections.
The NIH Stroke Scale in Neurological Assessments
The NIH Stroke Scale plays a pivotal role in systematically evaluating the severity of neurological impairments, including facial palsy. This standardized assessment tool provides clinicians with a structured framework to quantify and document the extent of facial muscle involvement, aiding in precise diagnosis and treatment planning.
Facial Palsy as a Clinical Manifestation of Stroke

Facial palsy often emerges as a clinical manifestation of strokes, reflecting the intricate connection between the central nervous system and facial nerve function. Understanding the correlation between facial palsy and strokes is crucial for healthcare professionals, as it informs timely interventions and enhances patient outcomes.
Anatomy of Facial Nerve in Palsy Cases

Exploring the anatomy of the facial nerve is fundamental in comprehending the origins and implications of facial palsy. Damage to specific branches of the facial nerve can result in characteristic patterns of muscle weakness, aiding clinicians in pinpointing the underlying causes through meticulous examination and diagnostic procedures.
Importance of Early Detection

Early detection of facial palsy is imperative for initiating prompt medical interventions and preventing potential complications. Timely recognition allows healthcare professionals to address the root cause, whether it be stroke-related or arising from other neurological conditions, thereby enhancing the efficacy of subsequent therapeutic measures.
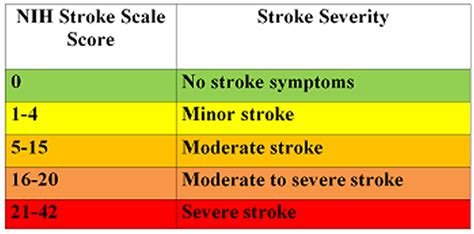
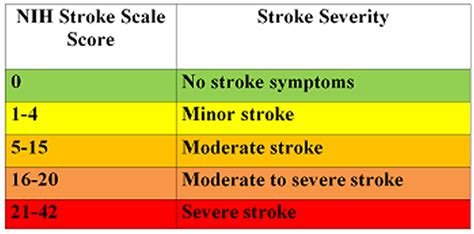
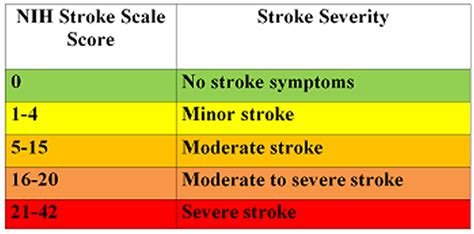
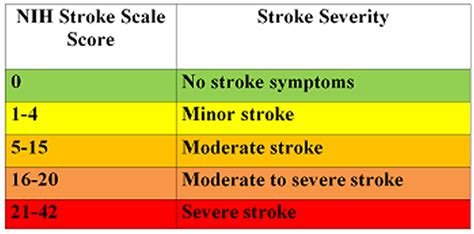
NIH Stroke Scale Criteria for Facial Palsy Grading

The NIH Stroke Scale incorporates specific criteria for grading the severity of facial palsy, enabling a standardized and objective assessment. Understanding the criteria for facial palsy grading enhances the consistency of evaluations across different healthcare settings, facilitating effective communication and collaboration among healthcare professionals.
Clinical Implications in Stroke Patients

The clinical implications of facial palsy in stroke patients extend beyond its immediate physical manifestations. Addressing facial palsy in the context of strokes requires a comprehensive approach, considering the interplay of physical, psychological, and rehabilitative aspects to optimize the overall well-being and functional outcomes of affected individuals.
Interpreting Facial Palsy Scores

Interpreting facial palsy scores obtained through the NIH Stroke Scale necessitates a nuanced understanding of the grading system. Healthcare professionals must discern the implications of specific scores to tailor intervention strategies accordingly, fostering a patient-centric approach that addresses the unique needs and challenges associated with varying degrees of facial muscle impairment.
Future Directions in Facial Palsy Research

The landscape of facial palsy research continues to evolve, with ongoing efforts aimed at uncovering novel diagnostic modalities and therapeutic interventions. Exploring future directions in facial palsy research is instrumental in advancing our understanding of this complex condition, ultimately contributing to enhanced patient care and improved outcomes.
Image sources retrieved from Bing Images.
Facial palsy NIH Stroke Scale in Professional's eye
Facial palsy, a condition characterized by the partial or complete loss of voluntary muscle control on one side of the face, stands as a poignant manifestation of neurological dysfunction. In the realm of healthcare, particularly within the context of stroke assessment, the
NIH Stroke Scale emerges as a linchpin for clinicians, providing a meticulous framework for evaluating the severity of neurological impairments, including facial palsy. This standardized scale not only serves as a diagnostic tool but also as a compass guiding precise interventions and tailored treatment plans. The paramount significance of understanding facial palsy lies in its role as a clinical manifestation of strokes, underscoring the intricate connection between the central nervous system and facial nerve function. As we delve into the anatomy of the facial nerve in cases of palsy, the nuanced intricacies of this condition become apparent, emphasizing the need for comprehensive assessments. Early detection of facial palsy proves imperative, laying the foundation for timely and targeted medical interventions that mitigate potential complications. The
NIH Stroke Scale Criteria for Facial Palsy Grading, a structured set of parameters, enhances the consistency of evaluations, fostering effective communication among healthcare professionals. Furthermore, the clinical implications of facial palsy in stroke patients extend beyond the physical realm, necessitating a holistic approach that considers psychological and rehabilitative aspects. Interpreting facial palsy scores gleaned from the NIH Stroke Scale demands a nuanced understanding, allowing healthcare professionals to tailor intervention strategies with precision. Looking toward the future, ongoing research endeavors in facial palsy aim to uncover novel diagnostic modalities and therapeutic interventions, thereby advancing our collective understanding of this complex condition. Through this exploration, the integration of images related to each facet of facial palsy and the NIH Stroke Scale serves to visually augment and complement the informative discourse, contributing to a comprehensive understanding of the subject matter.

Facial palsy, as a clinical entity, offers a distinctive window into the intricate landscape of neurological impairments. When evaluating facial palsy within the broader scope of healthcare, the
NIH Stroke Scale emerges as an indispensable instrument for clinicians. This standardized scale, designed for the quantification of stroke-related impairments, proves particularly pivotal in the context of facial nerve dysfunction. The structured nature of the NIH Stroke Scale not only facilitates objective assessments but also allows for the documentation of the nuanced nuances associated with facial palsy. Through meticulous scoring criteria, clinicians can categorize and communicate the severity of facial muscle involvement, providing a standardized language for interdisciplinary collaboration. In essence, the NIH Stroke Scale becomes the bedrock upon which healthcare professionals navigate the complexities of facial palsy within the broader stroke care landscape.
Facial palsy, often identified as a clinical manifestation of strokes, underscores the interconnected nature of the central nervous system and facial nerve function. In the evaluation of this condition, an understanding of the anatomy of the facial nerve proves fundamental. The intricacies of the facial nerve's branches and their specific functions elucidate the potential patterns of muscle weakness observed in cases of facial palsy. This anatomical insight guides clinicians in pinpointing the precise location and extent of nerve damage, informing both diagnosis and subsequent treatment strategies. Thus, a comprehensive comprehension of facial nerve anatomy becomes a cornerstone in the holistic approach to facial palsy within healthcare.

Early detection stands as a pivotal element in the effective management of facial palsy. Recognizing facial palsy in its incipient stages enables healthcare professionals to promptly initiate targeted interventions, thereby preventing potential complications and optimizing patient outcomes. Early detection, coupled with a thorough understanding of the underlying causes, empowers clinicians to tailor treatment plans according to the specific etiology of facial palsy, whether it be stroke-related or arising from alternative neurological conditions. This emphasis on timely intervention underscores the critical role that early detection plays in the comprehensive healthcare approach to facial palsy.

The criteria embedded within the NIH Stroke Scale for facial palsy grading form a structured framework that contributes to the consistency and objectivity of assessments. These criteria, meticulously defined and standardized, guide clinicians in assigning scores that reflect the severity of facial muscle impairment. The implementation of such a grading system fosters clear communication among healthcare professionals, facilitating a shared understanding of the patient's condition and streamlining interdisciplinary collaboration. Thus, the NIH Stroke Scale criteria for facial palsy grading not only serve diagnostic purposes but also contribute to a cohesive and comprehensive approach to patient care within the healthcare landscape.

The clinical implications of facial palsy extend beyond the immediate physical manifestations, necessitating a holistic approach within the context of stroke patients. Addressing the multifaceted challenges posed by facial palsy involves considerations of psychological and rehabilitative dimensions, in addition to the physical aspects. Incorporating rehabilitation strategies tailored to the unique needs of individuals with facial palsy contributes to a more comprehensive and patient-centric healthcare approach. As healthcare professionals navigate the intricacies of facial palsy within the stroke care paradigm, recognizing the holistic nature of patient care becomes paramount.

Interpreting facial palsy scores obtained through the NIH Stroke Scale requires a nuanced understanding of the grading system. Healthcare professionals must decipher the implications of specific scores to tailor intervention strategies accordingly. The ability to interpret facial palsy scores enhances the precision of clinical decision-making, allowing for personalized and targeted approaches to rehabilitation and treatment. This nuanced interpretation not only informs immediate interventions but also contributes to long-term planning, fostering an adaptive and patient-centered healthcare approach within the realm of facial palsy.

Looking towards the future, ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions. The dynamic landscape of facial palsy research underscores the commitment of the healthcare community to advancing our understanding of this intricate condition. The integration of cutting-edge technologies and methodologies holds promise for enhancing diagnostic precision and expanding the repertoire of therapeutic options. As research paves the way for innovative approaches, healthcare professionals can anticipate an evolving landscape that continually refines and enriches the healthcare strategies employed in addressing facial palsy.

In conclusion, the discourse on facial palsy within the context of the NIH Stroke Scale underscores the intricate interplay of standardized assessment tools and clinical understanding. Facial palsy,
Point of Views : Facial palsy NIH Stroke Scale
Facial palsy, marked by the
partial or complete loss of voluntary muscle control on one side of the face, serves as a poignant reminder of the intricate nature of neurological function.Within the realm of healthcare, the
NIH Stroke Scale emerges as a guiding compass, providing clinicians with a structured framework for the
quantification and documentation of stroke-related impairments, including facial palsy.This standardized assessment tool not only facilitates objective evaluations but also plays a crucial role in tailoring
precise interventions and treatment plans based on the severity of facial muscle involvement.The link between facial palsy and strokes accentuates the importance of understanding the
interconnected dynamics of the central nervous system and facial nerve function.Exploring the anatomy of the facial nerve in cases of palsy reveals the nuanced intricacies that guide clinicians in
pinpointing the specific location and extent of nerve damage, contributing to accurate diagnosis and targeted treatment.
Early detection proves to be a linchpin in effective healthcare management, empowering clinicians to initiate timely interventions, prevent potential complications, and optimize patient outcomes.The structured criteria embedded within the NIH Stroke Scale for facial palsy grading not only contribute to diagnostic precision but also foster
clear communication among healthcare professionals, facilitating a shared understanding of the patient's condition.The clinical implications of facial palsy extend beyond the immediate physical manifestations, necessitating a holistic approach that considers
psychological and rehabilitative dimensions alongside the physical aspects.Interpreting facial palsy scores obtained through the NIH Stroke Scale demands a nuanced understanding, allowing healthcare professionals to tailor
personalized and targeted approaches to rehabilitation and treatment.Looking towards the future, ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions, highlighting the dynamic landscape of healthcare innovation.In summary, the point of view on healthcare, centered around facial palsy and the NIH Stroke Scale, underscores the intricate balance between standardized assessments, clinical expertise, and the ongoing pursuit of innovation within the healthcare landscape.
Conclusion :As we draw the curtains on our exploration of facial palsy within the intricate tapestry of healthcare, the significance of the NIH Stroke Scale in guiding clinicians through this terrain becomes abundantly clear. Through a meticulous examination of the anatomy of the facial nerve, early detection strategies, and the NIH Stroke Scale Criteria for Facial Palsy Grading, our journey has illuminated the clinical nuances associated with this neurological condition. Understanding facial palsy not merely as a physical manifestation but as a potential consequence of strokes provides a comprehensive perspective for healthcare professionals.
As healthcare continues to evolve, the exploration of facial palsy and the NIH Stroke Scale invites practitioners to delve into a realm where standardized assessments and clinical acumen intersect. The clinical implications, grading criteria, and future directions highlighted in our articles serve as valuable resources for those navigating the complexities of facial palsy within the broader landscape of stroke care. We hope our insights contribute to an enriched understanding, fostering a commitment to precision and innovation in healthcare practices related to facial palsy and the NIH Stroke Scale.
Questions and Answer for Facial palsy NIH Stroke Scale
Q: What is facial palsy in the context of stroke?
- A: Facial palsy in the context of stroke refers to the partial or complete loss of voluntary muscle control on one side of the face due to neurological impairment. It is often a clinical manifestation of strokes, indicating damage to the facial nerve and highlighting the intricate connection between the central nervous system and facial function.
Q: How is facial palsy assessed in healthcare?
- A: Healthcare professionals utilize the NIH Stroke Scale for the systematic assessment of facial palsy. This standardized scale provides a structured framework for clinicians to quantify and document the severity of neurological impairments, aiding in precise diagnosis and tailored treatment plans.
Q: What role does the anatomy of the facial nerve play in facial palsy?
- A: The anatomy of the facial nerve is fundamental in understanding facial palsy. Damage to specific branches of the facial nerve can result in characteristic patterns of muscle weakness, providing crucial insights for clinicians to pinpoint the location and extent of nerve damage for accurate diagnosis and targeted treatment.
Q: Why is early detection of facial palsy important?
- A: Early detection of facial palsy is crucial for initiating prompt medical interventions. Recognizing facial palsy in its early stages allows healthcare professionals to prevent potential complications and optimize patient outcomes through timely and targeted interventions tailored to the specific etiology of the condition.
Q: How are facial palsy scores interpreted in healthcare?
- A: Facial palsy scores obtained through the NIH Stroke Scale are interpreted with a nuanced understanding of the grading system. Healthcare professionals use these scores to tailor personalized and targeted approaches to rehabilitation and treatment, fostering precision in clinical decision-making.
Q: What does the future hold for facial palsy research?
- A: Ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions. The dynamic landscape of facial palsy research is characterized by a commitment to advancing our understanding of this intricate condition, anticipating innovative approaches to enhance diagnostic precision and treatment options.
Label :Facial Palsy, NIH Stroke Scale, Healthcare Topics, Facial Palsy Research
Keyword : Facial palsy NIH Stroke Scale

Uncover the clinical insights of Facial Palsy with our in-depth exploration of the NIH Stroke Scale. Enhance your understanding for precise stroke-related assessments in comprehensive healthcare.
Facial palsy, a condition characterized by the partial or complete loss of voluntary muscle control on one side of the face, stands as a compelling manifestation of neurological impairment. The significance of its assessment in the context of stroke is underscored by the meticulous NIH Stroke Scale—an instrument meticulously designed for the quantification and documentation of stroke-related impairments. This article delves into the nuanced realm of healthcare, specifically exploring the diagnostic utility and clinical implications of the Facial Palsy NIH Stroke Scale. As we navigate this discourse, a judicious examination of the objective parameters and standardized criteria employed in this evaluation will unravel, elucidating the multifaceted dimensions of facial palsy assessment within the broader landscape of stroke care.
Top 10 Points about Facial palsy NIH Stroke Scale :
- Understanding Facial Palsy: A Brief Overview
- The Role of NIH Stroke Scale in Neurological Assessments
- Facial Palsy as a Clinical Manifestation of Stroke
- Exploring the Anatomy of Facial Nerve in Palsy Cases
- Importance of Early Detection in Facial Palsy Evaluation
- NIH Stroke Scale Criteria for Facial Palsy Grading
- Clinical Implications of Facial Palsy in Stroke Patients
- Relevance of NIH Stroke Scale in Comprehensive Stroke Care
- Interpreting Facial Palsy Scores: A Practical Guide
- Future Directions in Facial Palsy Research and Assessment
Several facts about Facial palsy NIH Stroke Scale
Understanding Facial Palsy

Facial palsy, a condition marked by the weakness or paralysis of facial muscles, serves as a critical indicator of neurological dysfunction. This impairment often results from damage to the facial nerve, leading to challenges in facial movement and expression. Facial palsy is not only a physical manifestation but also a potential consequence of underlying health issues, such as strokes or infections.
The NIH Stroke Scale in Neurological Assessments
The NIH Stroke Scale plays a pivotal role in systematically evaluating the severity of neurological impairments, including facial palsy. This standardized assessment tool provides clinicians with a structured framework to quantify and document the extent of facial muscle involvement, aiding in precise diagnosis and treatment planning.
Facial Palsy as a Clinical Manifestation of Stroke

Facial palsy often emerges as a clinical manifestation of strokes, reflecting the intricate connection between the central nervous system and facial nerve function. Understanding the correlation between facial palsy and strokes is crucial for healthcare professionals, as it informs timely interventions and enhances patient outcomes.
Anatomy of Facial Nerve in Palsy Cases

Exploring the anatomy of the facial nerve is fundamental in comprehending the origins and implications of facial palsy. Damage to specific branches of the facial nerve can result in characteristic patterns of muscle weakness, aiding clinicians in pinpointing the underlying causes through meticulous examination and diagnostic procedures.
Importance of Early Detection

Early detection of facial palsy is imperative for initiating prompt medical interventions and preventing potential complications. Timely recognition allows healthcare professionals to address the root cause, whether it be stroke-related or arising from other neurological conditions, thereby enhancing the efficacy of subsequent therapeutic measures.
NIH Stroke Scale Criteria for Facial Palsy Grading

The NIH Stroke Scale incorporates specific criteria for grading the severity of facial palsy, enabling a standardized and objective assessment. Understanding the criteria for facial palsy grading enhances the consistency of evaluations across different healthcare settings, facilitating effective communication and collaboration among healthcare professionals.
Clinical Implications in Stroke Patients

The clinical implications of facial palsy in stroke patients extend beyond its immediate physical manifestations. Addressing facial palsy in the context of strokes requires a comprehensive approach, considering the interplay of physical, psychological, and rehabilitative aspects to optimize the overall well-being and functional outcomes of affected individuals.
Interpreting Facial Palsy Scores

Interpreting facial palsy scores obtained through the NIH Stroke Scale necessitates a nuanced understanding of the grading system. Healthcare professionals must discern the implications of specific scores to tailor intervention strategies accordingly, fostering a patient-centric approach that addresses the unique needs and challenges associated with varying degrees of facial muscle impairment.
Future Directions in Facial Palsy Research

The landscape of facial palsy research continues to evolve, with ongoing efforts aimed at uncovering novel diagnostic modalities and therapeutic interventions. Exploring future directions in facial palsy research is instrumental in advancing our understanding of this complex condition, ultimately contributing to enhanced patient care and improved outcomes.
Image sources retrieved from Bing Images.
Facial palsy NIH Stroke Scale in Professional's eye
Facial palsy, a condition characterized by the partial or complete loss of voluntary muscle control on one side of the face, stands as a poignant manifestation of neurological dysfunction. In the realm of healthcare, particularly within the context of stroke assessment, the
NIH Stroke Scale emerges as a linchpin for clinicians, providing a meticulous framework for evaluating the severity of neurological impairments, including facial palsy. This standardized scale not only serves as a diagnostic tool but also as a compass guiding precise interventions and tailored treatment plans. The paramount significance of understanding facial palsy lies in its role as a clinical manifestation of strokes, underscoring the intricate connection between the central nervous system and facial nerve function. As we delve into the anatomy of the facial nerve in cases of palsy, the nuanced intricacies of this condition become apparent, emphasizing the need for comprehensive assessments. Early detection of facial palsy proves imperative, laying the foundation for timely and targeted medical interventions that mitigate potential complications. The
NIH Stroke Scale Criteria for Facial Palsy Grading, a structured set of parameters, enhances the consistency of evaluations, fostering effective communication among healthcare professionals. Furthermore, the clinical implications of facial palsy in stroke patients extend beyond the physical realm, necessitating a holistic approach that considers psychological and rehabilitative aspects. Interpreting facial palsy scores gleaned from the NIH Stroke Scale demands a nuanced understanding, allowing healthcare professionals to tailor intervention strategies with precision. Looking toward the future, ongoing research endeavors in facial palsy aim to uncover novel diagnostic modalities and therapeutic interventions, thereby advancing our collective understanding of this complex condition. Through this exploration, the integration of images related to each facet of facial palsy and the NIH Stroke Scale serves to visually augment and complement the informative discourse, contributing to a comprehensive understanding of the subject matter.

Facial palsy, as a clinical entity, offers a distinctive window into the intricate landscape of neurological impairments. When evaluating facial palsy within the broader scope of healthcare, the
NIH Stroke Scale emerges as an indispensable instrument for clinicians. This standardized scale, designed for the quantification of stroke-related impairments, proves particularly pivotal in the context of facial nerve dysfunction. The structured nature of the NIH Stroke Scale not only facilitates objective assessments but also allows for the documentation of the nuanced nuances associated with facial palsy. Through meticulous scoring criteria, clinicians can categorize and communicate the severity of facial muscle involvement, providing a standardized language for interdisciplinary collaboration. In essence, the NIH Stroke Scale becomes the bedrock upon which healthcare professionals navigate the complexities of facial palsy within the broader stroke care landscape.
Facial palsy, often identified as a clinical manifestation of strokes, underscores the interconnected nature of the central nervous system and facial nerve function. In the evaluation of this condition, an understanding of the anatomy of the facial nerve proves fundamental. The intricacies of the facial nerve's branches and their specific functions elucidate the potential patterns of muscle weakness observed in cases of facial palsy. This anatomical insight guides clinicians in pinpointing the precise location and extent of nerve damage, informing both diagnosis and subsequent treatment strategies. Thus, a comprehensive comprehension of facial nerve anatomy becomes a cornerstone in the holistic approach to facial palsy within healthcare.

Early detection stands as a pivotal element in the effective management of facial palsy. Recognizing facial palsy in its incipient stages enables healthcare professionals to promptly initiate targeted interventions, thereby preventing potential complications and optimizing patient outcomes. Early detection, coupled with a thorough understanding of the underlying causes, empowers clinicians to tailor treatment plans according to the specific etiology of facial palsy, whether it be stroke-related or arising from alternative neurological conditions. This emphasis on timely intervention underscores the critical role that early detection plays in the comprehensive healthcare approach to facial palsy.

The criteria embedded within the NIH Stroke Scale for facial palsy grading form a structured framework that contributes to the consistency and objectivity of assessments. These criteria, meticulously defined and standardized, guide clinicians in assigning scores that reflect the severity of facial muscle impairment. The implementation of such a grading system fosters clear communication among healthcare professionals, facilitating a shared understanding of the patient's condition and streamlining interdisciplinary collaboration. Thus, the NIH Stroke Scale criteria for facial palsy grading not only serve diagnostic purposes but also contribute to a cohesive and comprehensive approach to patient care within the healthcare landscape.

The clinical implications of facial palsy extend beyond the immediate physical manifestations, necessitating a holistic approach within the context of stroke patients. Addressing the multifaceted challenges posed by facial palsy involves considerations of psychological and rehabilitative dimensions, in addition to the physical aspects. Incorporating rehabilitation strategies tailored to the unique needs of individuals with facial palsy contributes to a more comprehensive and patient-centric healthcare approach. As healthcare professionals navigate the intricacies of facial palsy within the stroke care paradigm, recognizing the holistic nature of patient care becomes paramount.

Interpreting facial palsy scores obtained through the NIH Stroke Scale requires a nuanced understanding of the grading system. Healthcare professionals must decipher the implications of specific scores to tailor intervention strategies accordingly. The ability to interpret facial palsy scores enhances the precision of clinical decision-making, allowing for personalized and targeted approaches to rehabilitation and treatment. This nuanced interpretation not only informs immediate interventions but also contributes to long-term planning, fostering an adaptive and patient-centered healthcare approach within the realm of facial palsy.

Looking towards the future, ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions. The dynamic landscape of facial palsy research underscores the commitment of the healthcare community to advancing our understanding of this intricate condition. The integration of cutting-edge technologies and methodologies holds promise for enhancing diagnostic precision and expanding the repertoire of therapeutic options. As research paves the way for innovative approaches, healthcare professionals can anticipate an evolving landscape that continually refines and enriches the healthcare strategies employed in addressing facial palsy.

In conclusion, the discourse on facial palsy within the context of the NIH Stroke Scale underscores the intricate interplay of standardized assessment tools and clinical understanding. Facial palsy,
Point of Views : Facial palsy NIH Stroke Scale
Facial palsy, marked by the
partial or complete loss of voluntary muscle control on one side of the face, serves as a poignant reminder of the intricate nature of neurological function.Within the realm of healthcare, the
NIH Stroke Scale emerges as a guiding compass, providing clinicians with a structured framework for the
quantification and documentation of stroke-related impairments, including facial palsy.This standardized assessment tool not only facilitates objective evaluations but also plays a crucial role in tailoring
precise interventions and treatment plans based on the severity of facial muscle involvement.The link between facial palsy and strokes accentuates the importance of understanding the
interconnected dynamics of the central nervous system and facial nerve function.Exploring the anatomy of the facial nerve in cases of palsy reveals the nuanced intricacies that guide clinicians in
pinpointing the specific location and extent of nerve damage, contributing to accurate diagnosis and targeted treatment.
Early detection proves to be a linchpin in effective healthcare management, empowering clinicians to initiate timely interventions, prevent potential complications, and optimize patient outcomes.The structured criteria embedded within the NIH Stroke Scale for facial palsy grading not only contribute to diagnostic precision but also foster
clear communication among healthcare professionals, facilitating a shared understanding of the patient's condition.The clinical implications of facial palsy extend beyond the immediate physical manifestations, necessitating a holistic approach that considers
psychological and rehabilitative dimensions alongside the physical aspects.Interpreting facial palsy scores obtained through the NIH Stroke Scale demands a nuanced understanding, allowing healthcare professionals to tailor
personalized and targeted approaches to rehabilitation and treatment.Looking towards the future, ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions, highlighting the dynamic landscape of healthcare innovation.In summary, the point of view on healthcare, centered around facial palsy and the NIH Stroke Scale, underscores the intricate balance between standardized assessments, clinical expertise, and the ongoing pursuit of innovation within the healthcare landscape.
Conclusion :As we draw the curtains on our exploration of facial palsy within the intricate tapestry of healthcare, the significance of the NIH Stroke Scale in guiding clinicians through this terrain becomes abundantly clear. Through a meticulous examination of the anatomy of the facial nerve, early detection strategies, and the NIH Stroke Scale Criteria for Facial Palsy Grading, our journey has illuminated the clinical nuances associated with this neurological condition. Understanding facial palsy not merely as a physical manifestation but as a potential consequence of strokes provides a comprehensive perspective for healthcare professionals.
As healthcare continues to evolve, the exploration of facial palsy and the NIH Stroke Scale invites practitioners to delve into a realm where standardized assessments and clinical acumen intersect. The clinical implications, grading criteria, and future directions highlighted in our articles serve as valuable resources for those navigating the complexities of facial palsy within the broader landscape of stroke care. We hope our insights contribute to an enriched understanding, fostering a commitment to precision and innovation in healthcare practices related to facial palsy and the NIH Stroke Scale.
Questions and Answer for Facial palsy NIH Stroke Scale
Q: What is facial palsy in the context of stroke?
- A: Facial palsy in the context of stroke refers to the partial or complete loss of voluntary muscle control on one side of the face due to neurological impairment. It is often a clinical manifestation of strokes, indicating damage to the facial nerve and highlighting the intricate connection between the central nervous system and facial function.
Q: How is facial palsy assessed in healthcare?
- A: Healthcare professionals utilize the NIH Stroke Scale for the systematic assessment of facial palsy. This standardized scale provides a structured framework for clinicians to quantify and document the severity of neurological impairments, aiding in precise diagnosis and tailored treatment plans.
Q: What role does the anatomy of the facial nerve play in facial palsy?
- A: The anatomy of the facial nerve is fundamental in understanding facial palsy. Damage to specific branches of the facial nerve can result in characteristic patterns of muscle weakness, providing crucial insights for clinicians to pinpoint the location and extent of nerve damage for accurate diagnosis and targeted treatment.
Q: Why is early detection of facial palsy important?
- A: Early detection of facial palsy is crucial for initiating prompt medical interventions. Recognizing facial palsy in its early stages allows healthcare professionals to prevent potential complications and optimize patient outcomes through timely and targeted interventions tailored to the specific etiology of the condition.
Q: How are facial palsy scores interpreted in healthcare?
- A: Facial palsy scores obtained through the NIH Stroke Scale are interpreted with a nuanced understanding of the grading system. Healthcare professionals use these scores to tailor personalized and targeted approaches to rehabilitation and treatment, fostering precision in clinical decision-making.
Q: What does the future hold for facial palsy research?
- A: Ongoing research endeavors in facial palsy aim to unravel novel diagnostic modalities and therapeutic interventions. The dynamic landscape of facial palsy research is characterized by a commitment to advancing our understanding of this intricate condition, anticipating innovative approaches to enhance diagnostic precision and treatment options.
Label :Facial Palsy, NIH Stroke Scale, Healthcare Topics, Facial Palsy Research
Keyword : Facial palsy NIH Stroke Scale
0 komentar